- What is Multiple System Atrophy (MSA)?
Multiple system atrophy (MSA) is a rare neurodegenerative disorder characterized by variable combination of Parkinsonism (slownesss, stiffness, tremors, imbalance), cerebellar impairment (inco-ordination in walking and using hands) and autonomic features (postural dizziness, blackouts, urinary urgency/dribbling …)
- Is Multiple System Atrophy (MSA) Same as Parkinson’s disease?
No, MSA is not as same as Parkinson’s disease. Albeit MSA and Parkinson’s disease are part of same group of diseases called synucleopathy, the underlying changes in brain and progression of disease symptoms are significantly different from each other. Even the treatment responses are quite varied in both the disorders.
- How Common is MSA and who are prone to develop it?
Multiple System Atrophy (MSA) is a rare disease, affecting potentially 15,000 to 50,000 Americans, including men and women and all racial groups. No specific data on Indian patients exist.
- What is the reason to develop Multiple System Atrophy?
The cause of MSA is unknown. The vast majority of cases are sporadic, meaning they occur at random. A distinguishing feature of MSA is the accumulation of the protein alpha-synuclein in glia, the cells that support nerve cells in the brain. These deposits of alpha-synuclein particularly occur in oligodendroglia, a type of cell that makes myelin (a coating on nerve cells that lets them conduct electrical signals rapidly). This protein also accumulates in Parkinson’s disease, but in nerve cells. Because they both have a buildup of alpha-synuclein in cells, MSA and Parkinson’s disease are sometimes referred to as synucleinopathies. A possible risk factor for the disease is variations in the synuclein gene SCNA, which provides instructions for the production of alpha-synuclein.
- Can MSA be passed from one generation to other?
Multiple System Atrophy (MSA) is a sporadic disease (which means its not hereditary). We don’t know much about how it affects only in certain set of people or what genetic factors play a role here. However, different set of genes are being investigated for possible cause.
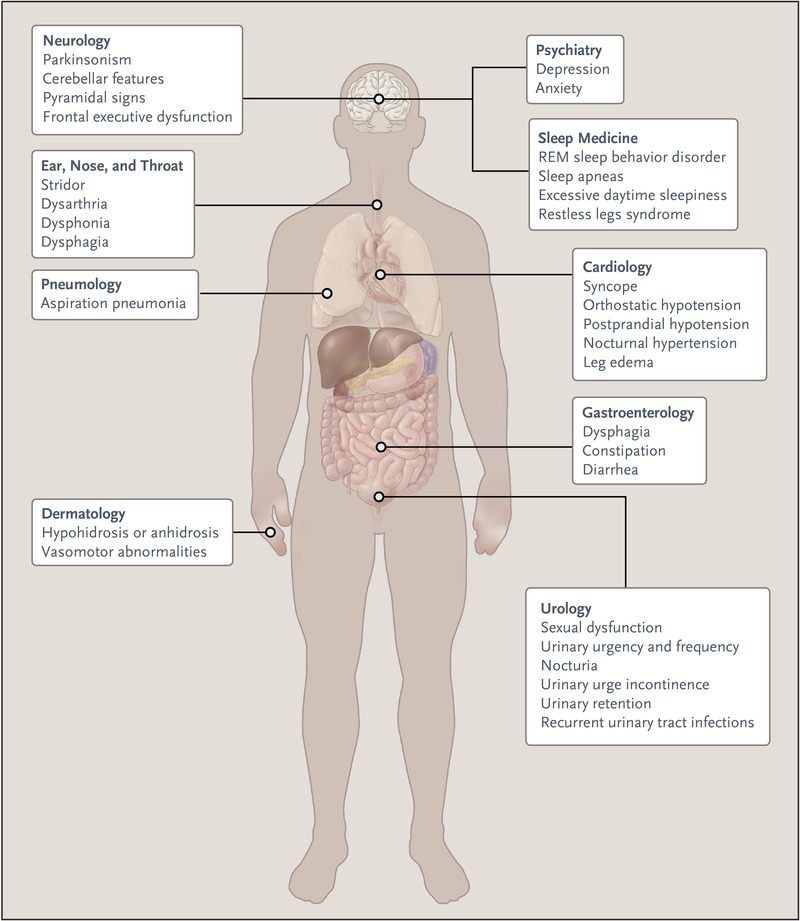
- What are the symptoms of MSA?
The initial symptoms of MSA are often difficult to distinguish from the initial symptoms of Parkinson’s disease and include:
- slowness of movement, tremor, or rigidity (stiffness)
- clumsiness or incoordination
- impaired speech, a croaky, quivering voice
- fainting or lightheadedness due to orthostatic hypotension, a condition in which blood pressure drops when rising from a seated or lying down position
- bladder control problems, such as a sudden urge to urinate or difficulty emptying the bladder
Doctors divide MSA into two different types, depending on the most prominent symptoms at the time an individual is evaluated:
- the parkinsonian type (MSA-P), with primary characteristics similar to Parkinson’s disease (such as moving slowly, stiffness, and tremor) along with problems of balance, coordination, and autonomic nervous system dysfunction
- the cerebellar type (MSA-C), with primary symptoms featuring ataxia (problems with balance and coordination), difficulty swallowing, speech abnormalities or a quavering voice, and abnormal eye movements (“cerebellar” reflects a part of the brain involved with coordination)
MSA tends to progress more rapidly than Parkinson’s disease, and most people with MSA will require an aid for walking, such as a cane or walker, within a few years after symptoms begin.
Additional symptoms of MSA include:
- contractures (chronic shortening of muscles or tendons around joints, which prevents the joints from moving freely) in the hands or limbs
- Pisa syndrome, an abnormal posture in which the body appears to be leaning to one side like the Leaning Tower of Pisa
- antecollis, in which the neck bends forward and the head drops down
- involuntary, uncontrollable sighing or gasping
- sleep disorders, including a tendency to act out dreams (called REM/ (Rapid Eye Movement sleep behavior disorder)
Some people with MSA may experience feelings of anxiety or depression.
- How is MSA diagnosed?
Making a diagnosis of Multiple system atrophy can be difficult, particularly in the early stages, in part because many of the features are similar to those observed in Parkinson’s disease.
After taking a clinical history and performing a brief neurological examination, a doctor may order a number of tests to help make the diagnosis. These tests might include autonomic testing (such as blood pressure control, heart rate control), assessment of bladder function, and/or neuroimaging such as an MRI (magnetic resonance imaging) or PET scan. An MRI of the brain may identify changes which might suggest MSA or rule out other causes of the observed symptoms.
- What are the treatment options for Multiple System Atrophy?
Currently, there are no treatments to delay the progressive neurodegeneration of MSA, and there is no cure. There are treatments to help people cope with the symptoms of MSA.
In some individuals, levodopa may improve motor function; however, the benefit may not continue as the disease progresses.
The fainting and lightheadedness from orthostatic hypotension may be treated with simple interventions such as wearing compression stockings, adding extra salt and/or water to the diet, and avoiding heavy meals. The drugs fludrocortisone and midodrine sometimes are prescribed.
Bladder control problems are treated according to the nature of the problem. Anticholinergic drugs, such as oxybutynin or tolteridine, may help reduce the sudden urge to urinate.
Fixed abnormal muscle postures (dystonia) may be controlled with injections of botulinum toxin.
Sleep problems such as REM sleep behavior disorder can be treated with medicines including clonazepam, melatonin, or some antidepressants.
Some individuals with MSA may have significant difficulties with swallowing and may need a feeding tube or nutritional support. Speech therapy may be helpful in identifying strategies to address swallowing difficulties.
Physical therapy helps maintain mobility, reduce contractures (chronic shortening of muscles or tendons around joints, which prevents the joints from moving freely), and decrease muscle spasms and abnormal posture.
Individuals may eventually need assistive devices such as walkers and wheelchairs. Occupational therapists help with home safety and learning new ways to address activities of daily living such as dressing and eating.
- What is the life expectancy of MSA?
Symptoms tend to appear in a person’s 50s and advance rapidly over the course of 5 to 10 years, with progressive loss of motor function and eventual confinement to bed.
- What are the support systems available for MSA?
Some of the online resources for MSA include