Falls are a significant concern for the elderly worldwide, affecting millions each year. As people age, the risk of falling increases due to various factors such as weakened muscles, poor balance, and chronic health conditions. According to the World Health Organization, falls are the second leading cause of accidental injury deaths globally, with seniors being the most vulnerable. These incidents often lead to severe injuries, reduced mobility, and a loss of independence, creating a substantial burden on healthcare systems and families. Understanding how to prevent and respond to falls is crucial in improving the quality of life for our aging population and aging disorders like Parkinson’s disease, Dementia, Arthritis, Visual issues etc. In this section we will see How to get up from a fall by yourself or How to assess and help someone who has fallen down.
What is a fall or how do we define a fall?
A fall is defined as an unexpected event where a person comes to rest on the ground or a lower level unintentionally. Falls can happen due to a variety of reasons, including tripping, slipping, or losing balance. For the elderly, factors like poor vision, muscle weakness, or medication side effects can increase the risk of falling. Recognizing and understanding the causes of falls is crucial in taking preventive measures to reduce their occurrence.
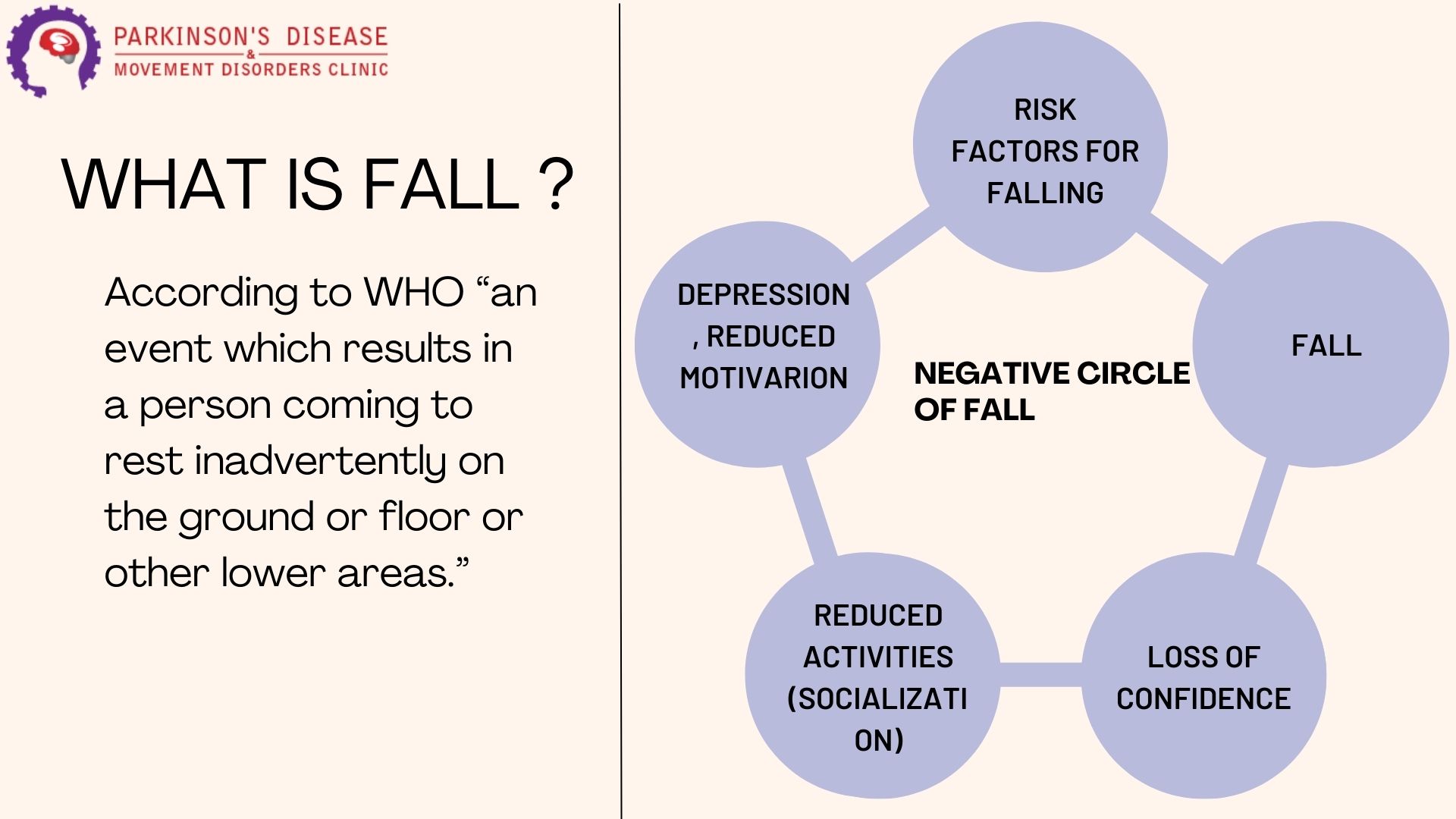
What is the negative circle of falls or the consequences of a fall?
The negative circle of falls refers to the cycle of adverse effects that can follow a fall, especially in the elderly. Consequences of a fall include physical injuries such as fractures or head trauma, which can lead to hospitalization and long-term disability. Beyond physical harm, falls can cause psychological impacts like fear of falling again, which often results in reduced activity levels. This inactivity can further weaken muscles and impair balance, increasing the likelihood of future falls. Additionally, falls can lead to a loss of independence and increased reliance on caregivers or family members, creating an emotional and financial burden. Breaking this cycle involves both effective fall prevention and appropriate response strategies when falls occur.
Who is prone for a fall?
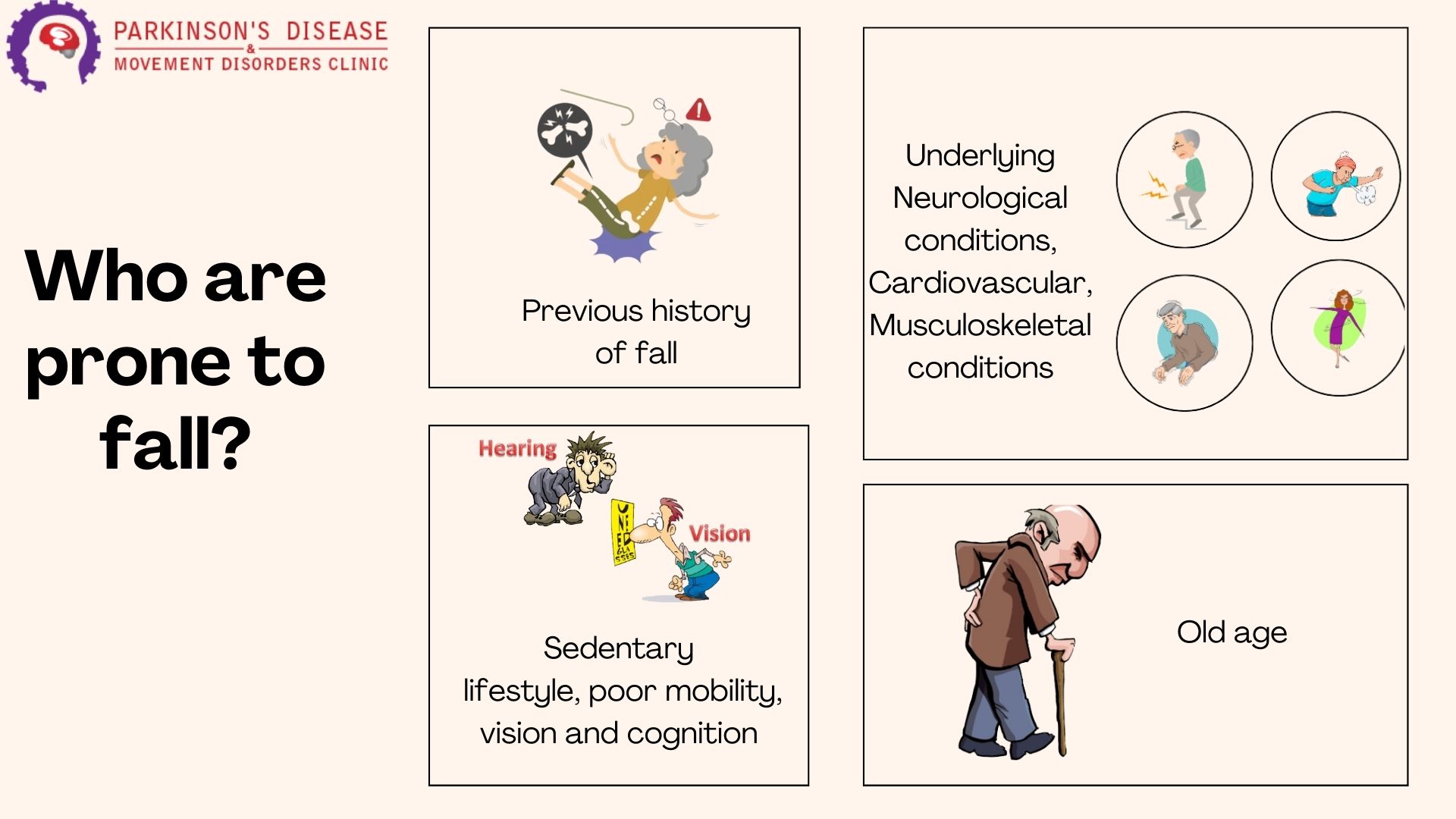
Several groups of people are particularly prone to falls, with the elderly being the most vulnerable. Key factors that increase the risk of falling include:
- Age: Older adults, especially those over 65, are at a higher risk due to age-related changes in balance, strength, and vision.
- Health Conditions: Chronic illnesses such as Parkinson’s disease, arthritis, and diabetes can impair mobility and balance, making falls more likely.
- Medications: Certain medications, especially those that affect the central nervous system (e.g., sedatives, antidepressants), can cause dizziness or drowsiness, increasing fall risk.
- Muscle Weakness: Decreased muscle strength, particularly in the legs, can make it harder to maintain balance.
- Poor Vision: Vision problems, such as cataracts or glaucoma, can affect depth perception and coordination.
- Environmental Hazards: Cluttered living spaces, poor lighting, and uneven flooring can create tripping hazards.
- History of Falls: Individuals who have fallen before are more likely to fall again due to a combination of physical and psychological factors.
Recognizing these risk factors is crucial for implementing effective fall prevention strategies.
What is a fall timeline and what are its stages?
A fall timeline outlines the stages and potential outcomes following a fall, particularly focusing on the elderly. The main stages include:
- Immediate Aftermath: This is the period right after the fall, where the individual may experience shock, pain, and confusion. Immediate medical assessment is crucial to determine any injuries.
- Delayed Initial Recovery: After the initial fall, some individuals may experience a slow recovery process. If person is lying down on floor after a fall beyond 10 min upto 59 mins is termed as delayed initial recovery. Factors such as existing health conditions, the severity of the fall, and inadequate immediate care can contribute to this delay. During this period, it is important to monitor for any signs of complications, such as internal injuries or worsening pain.
- Long Lie: This occurs when a person is unable to get up after a fall and remains on the ground for an extended period (Beyond 60 minutes), often due to a lack of strength, severe injury, or not being discovered promptly. A long lie can lead to serious health issues like dehydration, hypothermia, pressure sores, and even muscle breakdown.
- Post-Fall Syndrome: This syndrome includes a range of symptoms that may develop after the fall, such as fear of falling again, reduced mobility, loss of confidence, and increased dependence on others. Post-fall syndrome can significantly impact the individual’s quality of life and increase the risk of future falls.
How to assess a person who has fallen down?
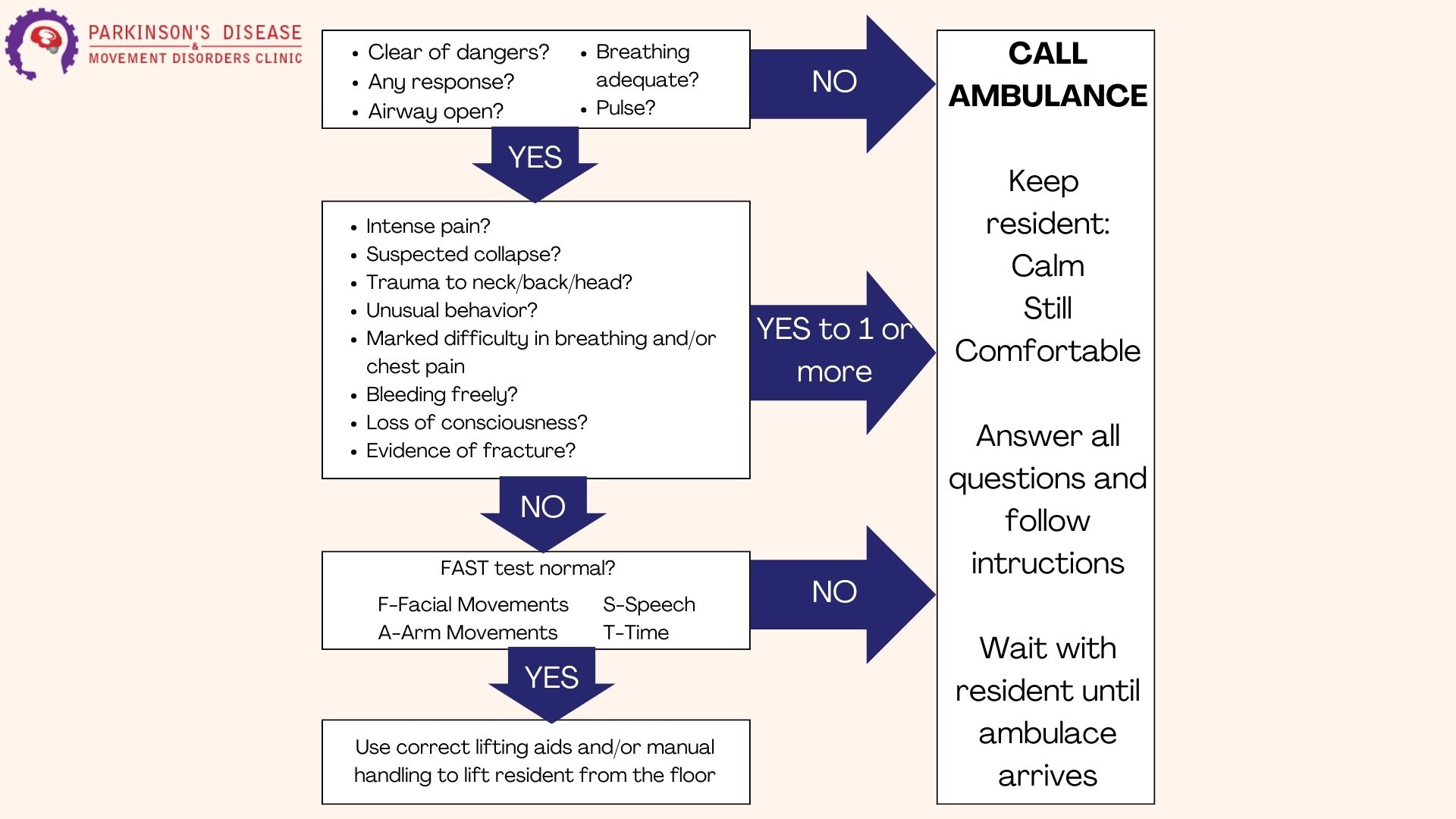
Assessing a person who has fallen down, especially an elderly individual, is crucial to determine the extent of their injuries and to provide the appropriate care. Here are the steps to follow:
- Stay Calm and Assess the Situation:
- Approach the person calmly and reassure them.
- Ensure the environment is safe to prevent further injury to the person or yourself.
- Check for Immediate Dangers:
- Look for any hazards that may have caused the fall, such as slippery floors or obstacles, and address them if possible.
- Initial Assessment:
- Consciousness: Check if the person is conscious and responsive.
- Breathing and Pulse: Ensure they are breathing and have a pulse. If there are any signs of severe injury or unconsciousness, call emergency services immediately.
- Check for Injuries:
- Head and Neck: Look for any signs of head or neck injuries. Do not move the person if you suspect a neck or spinal injury.
- Bones and Joints: Examine for any visible deformities, swelling, or bruising that could indicate fractures or sprains.
- Pain: Ask the person where they feel pain and observe their ability to move each limb without discomfort.
- Help Them Sit Up Slowly:
- If there are no severe injuries and they are able to, help them sit up slowly. This helps in assessing their balance and any delayed pain responses.
- Get Help if Needed:
- If the person cannot get up by themselves, do not force them. Call for help from another person or emergency services if needed.
- Provide Comfort and Reassurance:
- Keep the person warm and comfortable while waiting for additional help or medical assistance.
- Stay with them and continue to reassure them to reduce anxiety and fear.
- Document the Incident:
- Take note of what happened, including the time of the fall, how it occurred, and any visible injuries. This information will be helpful for medical professionals and caregivers.
- Follow Up:
- Even if the person appears uninjured, it is important to follow up with a healthcare provider to ensure there are no hidden injuries or complications.
By following these steps, you can provide appropriate immediate care and help ensure the safety and well-being of a person who has fallen.
How can I get up safely after a fall, and how can someone help me if I can't get up by myself?
In the provided video demonstration, you will see step-by-step instructions on how to get up safely after a fall, whether you are starting from a sitting position or lying down. The video also shows how someone can assist you if you are unable to get up on your own. Here are the key points covered in the video:
Getting Up by Yourself from a Sitting Position:
- Stay Calm: Take a moment to catch your breath and stay calm.
- Assess for Injuries: Check yourself for any pain or injuries before attempting to move.
- Find a Stable Support: Look around for a sturdy piece of furniture, like a chair or a sofa, that you can use to help you stand.
- Position Yourself: Move onto your hands and knees if possible. Crawl to the nearest stable support.
- Use Support to Rise: Place your hands on the support, bring one foot forward so you are in a kneeling position, and then push up with your legs to stand up slowly.
- Sit Down and Rest: Once you are up, sit down immediately on a stable chair to rest and assess any pain or discomfort.
Getting Up by Yourself from a Lying Down Position:
- Roll onto Your Side: Carefully roll onto your side to prevent straining your back.
- Get onto Hands and Knees: Push yourself onto your hands and knees.
- Crawl to Support: Crawl to a sturdy piece of furniture that you can use to help you stand.
- Kneel and Push Up: Place your hands on the support, bring one knee up, and push up with your arms and legs to stand up slowly.
- Rest and Assess: Sit down on a stable chair to rest and check for any injuries or pain.
Assisting Someone Else to Get Up:
- Stay Calm and Reassure: Approach the person calmly and reassure them.
- Check for Injuries: Gently ask if they feel any pain and check for obvious injuries.
- Find a Sturdy Support: Ensure there is stable furniture nearby that they can use to help them get up.
- Assist to Hands and Knees: Help them roll onto their side and then onto their hands and knees.
- Guide to Support: Guide them to crawl to the nearest support.
- Support Them to Stand: Stand close by to offer support as they use the furniture to help themselves stand up. Do not lift them directly, as this could cause further injury to both you and them.
- Sit and Rest: Once they are standing, assist them to sit on a stable chair to rest and assess for any pain or discomfort.
These steps, demonstrated in the video, provide practical guidance on how to safely get up after a fall and how to assist someone else. Always prioritize safety and seek medical attention if there
