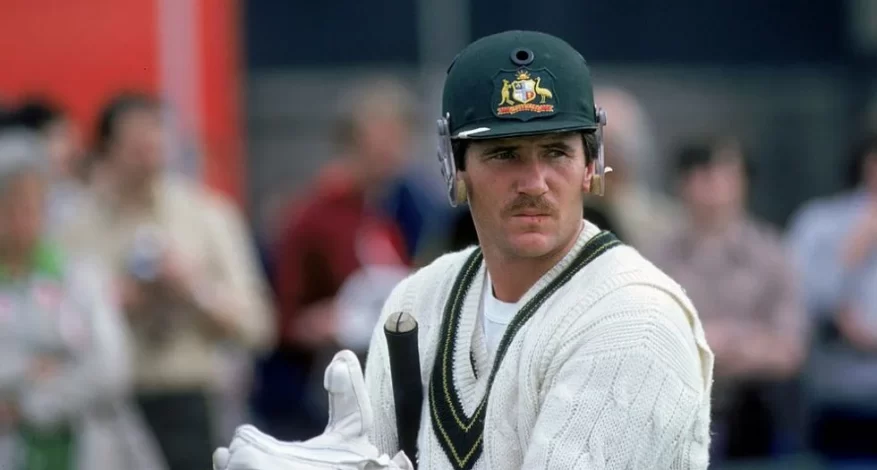
Australian Cricket Legend Allan Border Opens Up About His Battle with Parkinson’s Disease
Allan Border, the former Australian cricket captain, has revealed that he has been battling Parkinson’s disease for the past seven years. Parkinson’s is a progressive disorder of the nervous system that affects movement and causes unintended or uncontrollable movements. Border was diagnosed with the disease in 2016 but chose to keep it private until now. Parkinson’s is an neurodegenrative / Ageing disease that causes progressive brain damage, with common symptoms of loss of muscle control, tremors, muscle rigidity, and slowness of movement. Border said that he will continue to fight the disease and that he is not scared about the immediate future. Border played 156 Tests between 1979 and 1994 – 93 of them as captain – and was the first batter to score 11,000 runs, finishing with 11,174. He also led Australia to victory in the 1987 World Cup and ended up playing 273 ODIs. Since retiring, he has served as an Australian selector and been a broadcast commentator.
Here are the top 5 questions on Parkinson’s Disease being queried on Google search and their answers:
- What is Parkinson’s disease (PD)?
– Parkinson’s disease is a progressive neurological disorder or disorder of the brain. It affects men slightly more than women and Caucasians more than people of color. The cause of PD is still not clearly understood, with theories including genetic, environmental, and viral factors.
- What are the symptoms of Parkinson’s disease?
– The most common symptoms of Parkinson’s disease include tremor at rest, rigidity (stiffness), bradykinesia (slowness of movement), and postural instability (lack of balance). Individuals with PD may also experience difficulty walking, reduced facial expressions, small handwriting, soft and muffled speech, constipation, sleep disturbances, depression, anxiety, memory problems, difficulty swallowing, and reduced armswing.
- How does Parkinson’s disease begin?
– The characteristic brain pathology and motor symptoms of Parkinson’s disease are well established, but the details of the disease’s cause and course are much murkier. Many scientists are searching for blood- or urine-based biomarkers, or imaging agents, that could objectively identify the risk of Parkinson’s, but so far no leading contender has emerged.
- What other specialists or healthcare professionals should help me manage my care?
– It is important to ask about the other health professionals who can help manage Parkinson’s disease. This may include physical therapists, occupational therapists, speech therapists, and social workers, among others[.
- Besides taking medications, what else can I do to manage my Parkinson’s disease? Are there specific therapies, exercises, or lifestyle changes that can help?
– In addition to medications, there are specific therapies, exercises, and lifestyle changes that can help manage Parkinson’s disease. These may include physical therapy, speech therapy, occupational therapy, and regular exercise, among other strategies.
These questions cover a range of important topics related to Parkinson’s disease, from understanding the condition and its symptoms to managing care and seeking additional support from healthcare professionals.
Citations:
[1] https://www.foxsports.com.au/cricket/australian-cricket-legend-allan-border-has-parkinsons-disease/news-story/c96d056bd549403184ec81a1ac66d72f
[2] https://youtube.com/watch?v=o51v2az8mgo
[3] https://www.smh.com.au/sport/cricket/allan-border-reveals-he-has-parkinsons-disease-20230630-p5dky9.html
[4] https://apnews.com/article/allan-border-cricket-ad78339b79c704dfb315b10100aba538
[5] https://www.espncricinfo.com/story/allan-border-reveals-he-has-parkinsons-disease-1385094
[6] https://www.movementdisordersclinic.com/
[7] https://www.apdaparkinson.org/article/common-questions-from-caregivers/
[8] https://www.nature.com/articles/538S17a
[9] https://www.parkinson.org/library/fact-sheets/questions-doctor-visit

Lets Learn About Progressive Supranuclear Palsy (PSP)

Progressive Supranuclear Palsy (PSP)
On October 19-20, 2023, a significant global event brought together leading specialists to address the pressing issues surrounding Progressive supranuclear palsy (PSP) in London, UK
Progressive supranuclear palsy (PSP) is a rare and complex neurodegenerative disorder.
Here are 10 important things to know about PSP:
- Rare Condition: PSP is a relatively uncommon condition, affecting approximately 5-6 people per 100,000 in the population.
- Onset and Age: It typically affects individuals in their 60s or 70s, but early-onset PSP can occur in individuals in their 40s or 50s.
- Motor Symptoms: PSP is characterized by motor difficulties, including stiffness, slowness of movement, and frequent falls. This can make it resemble Parkinson’s disease, but PSP has distinct features.
- Eye Movement Problems: One of the hallmark features of PSP is difficulty controlling eye movements, leading to issues with looking up and down. This can cause falls and difficulty with balance.
- Cognitive Changes: Individuals with PSP may experience cognitive changes, such as difficulties with memory, decision-making, and problem-solving. However, these changes are usually less severe than those seen in Alzheimer’s disease.
- Behavioral and Emotional Changes: PSP can lead to changes in behavior and emotions, including irritability, apathy, and mood swings.
- Speech and Swallowing Issues: Speech problems, such as slurred speech, and difficulties with swallowing are common in PSP.
- No Cure: Currently, there is no cure for PSP. Treatment primarily focuses on managing symptoms and improving the patient’s quality of life.
- Abnormal Brain Protein: PSP is associated with the buildup of an abnormal protein called tau in specific areas of the brain. This protein accumulation is a key feature in diagnosing the condition.
- Diagnosis Challenges: Diagnosing PSP can be challenging because its symptoms overlap with other neurological disorders, like Parkinson’s disease. A definitive diagnosis often requires a combination of clinical evaluation, medical history, and specific neurological tests.
Supportive Care: PSP patients benefit from a multidisciplinary approach involving neurologists, physical therapists, occupational therapists, and speech therapists. Supportive care and therapy focus on symptom management and maintaining the patient’s quality of life. CurePSP and PSPA (Progressive Supranuclear Palsy Association) are two organizations dedicated to supporting individuals and families affected by Progressive supranuclear palsy (PSP) and related disorders
It’s important to note that PSP is a progressive and challenging condition that can significantly impact a person’s quality of life. Raising awareness and understanding of the disease is crucial for providing better care and support for individuals living with PSP and their families.
www.movementdisordersclinic.com
Bangalore, India
Appointments : +91 7026603300
Join our Whatsapp Channel for similar information: https://whatsapp.com/channel/0029Va53s2N3bbVCdsUkKz2n
Stigma in Parkinson Disease : How to overcome it

What is Stigma in Parkinson Disease? What are the types of Stigma?
Stigma in Parkinson’s disease, like many other chronic medical conditions, is a significant challenge that individuals with the condition and their families face. Stigma can be broadly categorized into seven types, as defined by Link and Phelan in their influential work on the subject. These seven types can help us understand how Parkinson’s disease is stigmatized and the impact it has on those affected.
Public Stigma: This type of stigma involves the negative beliefs, attitudes, and stereotypes held by society at large towards people with Parkinson’s disease. These attitudes can manifest as fear, misunderstanding, or avoidance. Public stigma can make it difficult for individuals with Parkinson’s disease to socialize or access the support they need.
Self-Stigma: Self-stigma refers to the internalization of the negative stereotypes and beliefs that society holds about Parkinson’s disease. People with Parkinson’s may start to believe these stereotypes and feel ashamed or inferior, which can lead to a decrease in self-esteem and overall well-being.
Structural Stigma: Structural stigma pertains to societal and institutional practices that discriminate against or disadvantage people with Parkinson’s disease. This can manifest in healthcare disparities, limited access to quality care, or difficulties in obtaining insurance coverage for treatment and support services.
Affiliated Stigma: Parkinson’s disease doesn’t just affect the individual diagnosed; it also has an impact on their family and caregivers. Affiliated stigma involves the negative attitudes and discrimination experienced by the family members and friends of someone with Parkinson’s. They may face judgment or feel isolated, which can strain their relationships and well-being.
Courtesy Stigma: Individuals who care for or interact with people living with Parkinson’s disease can also face courtesy stigma. This occurs when people are treated unfairly or with disrespect because of their association with someone who has the condition. Healthcare providers, for instance, may experience this form of stigma.
Label Avoidance: Label avoidance stigma refers to individuals’ reluctance to be identified as having Parkinson’s disease due to the negative consequences they anticipate, such as potential discrimination or social rejection. This can lead to people avoiding diagnosis and treatment, which may result in delayed intervention and poorer outcomes.
Perceived Stigma: Perceived stigma is the fear or anticipation of experiencing stigma based on one’s condition. People with Parkinson’s may anticipate discrimination or negative reactions from others, which can lead to anxiety, depression, or reluctance to seek social support.
Addressing stigma in Parkinson’s disease is crucial to improving the lives of those affected. This can be accomplished through a combination of education, awareness campaigns, and policy changes. Increased public understanding and empathy can help reduce public stigma, while empowering individuals with Parkinson’s to share their stories and experiences can combat self-stigma. Moreover, healthcare systems and institutions should work to reduce structural stigma and ensure equitable access to care.
In conclusion, understanding the seven types of stigma in Parkinson’s disease provides a comprehensive framework for addressing the complex challenges faced by individuals with the condition and their loved ones. By actively working to reduce these stigmas, we can create a more inclusive and supportive environment for those living with Parkinson’s disease.
How to overcome Parkinson Disease Stigma?

Reducing stigma in Parkinson disease is essential to improving the quality of life for individuals affected by the condition. Stigma can have a profound impact on mental health, social relationships, and access to healthcare. Here are some strategies and approaches to reduce stigma in Parkinson’s disease:
A. Education and Awareness:
Public education campaigns: Conduct public awareness campaigns to provide accurate information about Parkinson’s disease. These campaigns can dispel myths and stereotypes, helping to increase understanding and empathy.
Schools and communities: Introduce educational programs about Parkinson’s disease in schools and local communities. Promoting understanding from a young age can foster a more accepting society.
Media and Representation:
Encourage accurate portrayal: Work with media outlets to ensure that depictions of Parkinson’s in movies, television, and news are accurate and respectful. Avoid sensationalizing the condition or using it for comedic effect.
Highlight positive stories: Share stories of individuals with Parkinson’s who have achieved remarkable accomplishments, demonstrating that the condition doesn’t define their entire life.
B. Open Dialogue:
Support groups: Create and promote support groups where people with Parkinson’s, their caregivers, and family members can share their experiences, challenges, and triumphs. Open dialogue can reduce self-stigma and affiliated stigma.
Personal testimonials: Encourage individuals with Parkinson’s to share their personal stories, either in person or through written or online platforms. Personal narratives can be powerful tools for challenging stereotypes.
Healthcare and Policy:
Equal access to care: Advocate for policies that ensure equitable access to healthcare services, including specialist care, therapies, and medications. Reducing structural stigma in the healthcare system is crucial.
Training for healthcare professionals: Offer training to healthcare providers to help them understand the physical and emotional challenges faced by people with Parkinson’s. This can improve patient-provider relationships and reduce courtesy stigma.
C. Language Matters:
Use person-first language: Encourage the use of person-first language, where the person is emphasized over the condition. Instead of saying “a Parkinson’s patient,” say “a person living with Parkinson’s.”
Avoid derogatory terms: Educate people about the importance of avoiding derogatory or insensitive language that perpetuates stereotypes.
D. Empower Advocacy:
Support advocacy organizations: Join or support organizations that advocate for the rights and well-being of people with Parkinson’s. These organizations often have the resources and platforms to combat stigma effectively.
Political engagement: Engage with policymakers to promote legislation that protects the rights and dignity of individuals living with Parkinson’s disease.
Mental Health Support:
Address the emotional impact: Acknowledge the emotional and psychological challenges associated with Parkinson’s and provide access to mental health support and resources. This can help individuals cope with self-stigma and perceived stigma.
E. Promote Inclusivity:
Encourage social inclusion: Promote social activities and events that are accessible and welcoming to people with Parkinson’s. Inclusive environments help reduce perceived stigma and encourage participation.
Celebrate Achievements:
Recognize achievements: Highlight the accomplishments of individuals living with Parkinson’s, showcasing their resilience and contributions to society.
Reducing stigma in Parkinson’s disease is an ongoing process that involves the collective efforts of individuals, healthcare providers, policymakers, and communities. By fostering understanding and empathy, dispelling misconceptions, and promoting inclusivity, we can create a more accepting and supportive environment for those living with Parkinson’s disease and work towards reducing the stigma in Parkinson disease.
World Movement Disorders Day
World Movement Disorders Day
Do you know what is “Movement Disorders”? Or Do you know what are the disorders treated by an “Movement Disorders Specialists”?. Some of us have heard about the name “Parkinson’s Disease”, but do you know who named this disorder as “Parkinson’s Disease”? To answer these questions and create awareness about Movement Disorders, the “International Parkinson’s and Movement Disorders Society” has initiated November 29th as “World Movement Disorders Day”. This year (2022) would be first world Movement Disorder’s Day and would be a platform to create awareness about Movement Disorders Globally.
Movement Disorders are a group of brain disorders, which leads to either abnormally excess or slowness of body movements and not related to any other body system involvement. For example unable to move leg due to a ‘Fracture’ is NOT an Movement Disorders, however, unable to easily move the same leg due to dysfunction in brain (more specifically basal ganglia) leading to “Parkinson’s Disease” is an “Movement Disorder”. The movement disorders are specific set of diseases which occur due to dysfunction in certain deep brain structures, called as Basal Ganglia and its various connections. The common symptoms of dysfunction of this part of brain causes – generalized slowness (Parkinsonism), shaking of body parts (tremors), imbalance sensation (ataxia /drunkard walking), tendency to fall, abnormal posturing of body parts (dystonia), unwanted excessive movements of different body parts (chorea, ballism,) etc. These symptoms can occur individually or can occur in various combinations, based upon which different disease names are suggested like, Parkinson’s Disease, Huntington’s Disease, Progressive Supranuclear Palsy (PSP), Wilson’s disease, Spinocerebellar ataxia etc. These disorders can occur due to various underlying causes varying from infections of brain, body metabolic changes (like high or low blood sugars), medication related side effects, allergic disease of brain (autoimmune diseases), tumors of the brain, stroke like events, genetic abnormalities and due to normal ageing process. The underlying cause decides the treatment and outcome of these treatment. For example, a person developing symptoms of Parkinsonism (Slowness, stiffness, tremors, walking changes) due to metabolic / acute drug related reaction can be completely cured with treating the metabolic changes or stopping the offending medication. However, development of Parkinsonism secondary to ageing / genetic process – Parkinson’s disease can be well managed with treatment similar to blood pressure and diabetes. Given that these disorders are due to changes in the brain, these disorders are managed by Neurologist who is further specialized in this field, and they are called as “Movement Disorders Specialists”.

The International Parkinson and Movement Disorders Society has chosen 29th November to be as World Movement Disorders Day to commemorate with birth anniversary of Prof. Jean-Martin Charcot (1825 – 1893). Prof. Jean-Martin Charcot was French Neurologist, born on 29th November 1825 in Paris. He has been referred as the ‘Father of French Neurology and one of the World’s Pioneers of Neurology’. He established Neurology clinic at the famous Salpetriere hospital in Paris, which was first of its kind then. His contributions are tremendous across the field of Medicine but much more to Neurology. His interests included hysteria and hypnotism. Dr. Charcot has various diseases / conditions / anatomical parts named after him (e.g: Charcot’s Artery, Charcot’s Joint, Charcot -Marie-Tooth Disease, Charcot’s Triad of Multiple Sclerosis etc). James Parkinson’s essay – “The Shaking Palsy”, which was written in 1817, was well recognized during the tenure of Charcot and was being known by the name of “Paralysis agitans”. Charcot lauded James Parkinson’s extensive descriptions and suggested that the disorder be named after him – “Parkinson’ Disease”. Hence, the term “Parkinson’s disease” came to existence in in later part of 19th century, due to Charcot’s recognition (la maladie de Parkinson). His extra ordinary contributions to field of Neurology and Movement disorders, has made International Parkinson and Movement Disorders Society to initiate World Movement Disorders Day to create awareness for all the movement disorders, albeit some of the major movement disorders have their own awareness days (e.g: April 11th – World Parkinson’s Disease Awareness day).

The Field of Movement disorders has been growing in India since the 2000’s and India has now its own movement disorders specialist’s society called as ‘Movement Disorders Society of India’, started in 2014. The number of movement disorders cases are on steady increase in India and the World Health Organization, has predicted a tremendous increase in Parkinson’s disease and other ageing disorders across India over the next decades. There is clear lack of systematic epidemiological studies to understand the prevalence of various movement disorders in India. Dr. Prashanth LK, Consultant Parkinson’s disease and Movement Disorders Specialist from Bangalore has worked with two other specialty Movement Disorders Clinic located in Mumbai and Kolkata to discuss the burden of movement disorders in India. In these specialized private movement disorders clinics, it has been noted that Parkinsonism disorders contributed to almost 2/3rd of the various diseases seen, which is followed by dystonic disorders (15%), and tremors (8%). The group also comment that among the Parkinsonian disorders, a trend of increase in atypical parkinsonism disorders are being on the raise and contributed to about 22% of the cohort. Given the variability of these disorders, and India needs to have its own research which can address these concerns. Some of the movement disorders are almost exclusive to India like the Spinocerebellar ataxia type-12 (also known as Aggarwal disease, as it is predominantly limited to this community) or some of the diseases are predominantly more here (like the Wilson’s disease, much more common in southern India due to increased consanguinity). To address these things awareness and support for research is required from all the stake holders. The Movement Disorders Specialists of India have formed consortium to address these specific issues and are trying to collaborate with other basic sciences fields to get in-house answers for problems which are exclusive for Indian community – Parkinson Research Alliance of India. In this context major pan India collaborative studies are going on diseases like Young Onset Parkinson’s Disease, Progressive Supranuclear Palsy with collaboration from Indian and International working groups. On the occasion of this first World Movement Disorders Awareness Day, lets spread the awareness of various movement disorders in India and need to encourage co-operative works with clinicians, scientists, philanthropists and patients to find answers to many of these rare and well known disorders.
Table : List of Few Common Movement Disorders and there understanding in simple English:
| Disease / Symptom name | Simple English interpretation |
| Parkinson’s Disease | Someone who is have a combination of slowness of body movement, stiffness of body, shaking/ tremors of hands and walking changes |
| Dystonia | Excess abnormal involuntary muscle contraction leading to posturing of the affected body parts (like neck = cervical dystonia, writing = writers cramp, jaw = jaw dystonia) |
| Tremors | Abnormal rhythmic shaking of a body part (hand = hand tremors, head = head tremors etc) |
| Huntington’s Disease | Someone have abnormally excessive, body movements, which are variable in intensity and duration. These people may also have behavioral / memory issues. |
| Blepharospasm | Excessive eye blinking and sometimes leading to closure of eyes |
| Hemifacial spasm | Abnormal intermittent facial contractions |
| Ataxia | Imbalance while walking (drunkard type walking) |
| Restless Leg Syndrome | Abnormal sensation of legs, especially during late evening / night, which improves/ reduced by walking around. |
| Tic | Abnormal repetitive body movements, which are due to satisfy once urge to do it (e.g, shoulder shrugging, jerking movements of head while speaking etc) |
| Progressive supranuclear palsy | Someone who is having symptoms of Parkinson’s disease, but also has significant balance issue leading to fall (especially backwards) |
A Sneak Peak into Gastrointestinal (GUT) Conundrum of Parkinson Disease
The understanding of Parkinson’s disease has been dramatically changing over the years. The gastrointestinal symptoms of Parkinson disease are well recognized and keeps on adding up to the number of symptoms of Non Motor Symptoms (NMS). Even further the question of whether Parkinson’s disease arises from Gut perse has become a promienent question among the scientists across the world. The has given raise to concept of GUT-BRAIN axis and further postulation of Gut first and Brain first theories. In this blog, we are trying to highlight the awareness about various gastrointestinal symptoms noted in patient with Parkinson’s disease.

The Gastrointestinal symptoms in Parkinson disease is one of the common NMS in PD, even early in the disease course. Several factors such as loss of dopaminergic activity, presence of Lewy bodies, gut exposure to neurotoxins, gut dysbiosis, cytokine-induced toxicity, inflammation-derived oxidative damage and aging have been associated with the pathogenesis and progression of PD although robust evidence is lacking.
Gastrointestinal Symptoms of in Parkinson Disease
The symptoms of Gut in Parkinson’s disease can be noted all the way from the mouth and salivary glands. the following list helps to understand the possible symptoms which could be associated with Parkinson’s disease.
Salivary Glands symptoms
- Reduced Saliva Production
- Low swallowing frequency leading to drooling
Mouth related symptoms
- Pooling of saliva and problems with movements needed to brush teeth can cause dental dysfunction
- Jaw tremors related discomfort
Pharynx related symptoms
- Oropharyngeal dysphagia increases risk of aspiration
Oesohagus related symptoms
- Slow esophageal transit
- Segmental esophageal spasm
- Spontaneous contractions of proximal esophagus
- Air trapping
- Aperistalsis
- Gastro-esophageal influx
Stomach symptoms
- Impaired gastric emptying causes nausea
- Bloating
- Early satiety and weight loss
Small Intestine symptoms
- Dilatation leading to bloating sensation
Colon symptoms
- Colonic dysmotility
- Constipation
- Megacolon
- Volvulus
- Bowel perforation
Rectum symptoms
- Anorectal dysfunction leads to difficulty with defecation
Management of Gastrointestinal symptoms in Parkinson disease

There are various symptomatic options for various GI related symptoms. The same has been highlighted in this article image.
Elephant in the Room – Astonishing Parkinson’s disease Beyond Tremors

The expression “Elephant in the room” is an metaphorical idiom used to describe something which everyone knows, but no one wants to mention or discuss it for various reasons. The above image is a part of “controversial art” by famous British artist Banksy. This art named “Elephant in the room” was featured as a part of US exhibition – “Barely legal” in 2006. It had it’s own set of controversies. However, the primary objective of this art was to highlight that billions of people lived below the poverty line. This art perse was a metaphor to speaking about elephant in the room and controversies there off.
Parkinson’s Disease is well known disorder where in people know issues about tremors, slowness, stiffness and walking related issues. However, there are many more other issues, which is well know to the patients, caregivers, and doctors, but most of the time, these symptoms are either brushed under the carpet or not enquired upon at consultation. Currently these features are becoming more important in the management of Parkinson’s Disease and more efforts are being put into the assessment and treatment of these issues. These are broadly classified under the category of Non Motor Symptoms (NMS) under the management of Parkinson’s Disease. However, these for all of us is the Elephant in the room which needs to be more outspoken and appropriate management needs to be done.
The International Parkinson Disease and Movement disorders society (IPMDS), has come up with exclusive scales on non motor symptoms to address this concern of elephant in the room.
“Elephant in the Room” – Parkinson’s Disease
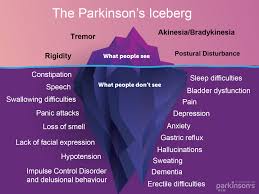
Image source: Parkinsonnsw
There are various symptoms which qualify for elephant in the room for Parkinson’s disease and prominent among them are
- Mood : All Parkinson’s disease patients might have some form of mood/behavioral changes, which is mostly under reported and only symptoms which become much bothersome are spoken about. Depression is one of the well know and needs to be tackled properly.
- Sleep : Sleep disturbances are common and sometimes predate the onset of motor symptoms by many years. These symptoms might include vivid dreams, nightmares, shouting/yelling/enacting in dreams (aka RBD), restless leg syndrome (RLS).
- Bladder issues : Urinary urgency, increased frequency, night time increased urinary frequency/volume are common bladder issues noted.
- Constipation : Constipation is probably one of well accepted and acknowledged symptom, which is noted well before the onset of motor symptoms
- Sexual dysfunction : Probably this is one of the least discussed non motor symptom, and mostly not addressed. The issue has to be discussed promptly by the patient or the doctor as its fairly treatable symptom
- Excessive sweating / drooling / skin oilyness : These changes are noted in patients with Parkinson’s disease and skin changes can be noted.
- Postural dizziness / fatigue : Patients with Parkinson’s disease tend to have
In the subsequent weeks, we will try to bring out exclusive write ups, including their symptoms, management, both on video and web write up. Effort will be put to get Kannada language audio/video files for the patients and care givers. Keep a lookout on the facebook page and youtube channel.
European Academy of Neurology Interview with Dr. Prashanth LK on COVID19 Impact

Prof. Elena Moro, Secretary General of European Academy of Neurology, had interview with Dr. Prashanth LK on COVID19 and its impact on medical practice at ground level. This is published in the the European Academy of Neurology (www.ean.org) EAN pages section
Brief excerpt of the interview with Dr. Prashanth LK is below and the rest can be accessed at the EAN Pages section (https://www.eanpages.org/2020/11/01/covid19-around-the-world-clinician-interviews-on-experience-and-impact-of-the-virus/).
1. How has COVID19 and national measures to control it affected routine and emergency neurology service delivery in your country? How have you adapted to deal with the impact?
The speed and rampage of COVID19 pandemic have paralysed every country in 2020. No matter what, the amount of measures taken at every level, appears to be miniscule in front of its wrath. The neurology community across India was gearing up for the COVID19 breakout but, the impact of COVID19 was beyond anyone’s perception until it hit upon us. The Annals of Indian Academy of Neurology (Official journal of Indian Academy of Neurology), came up with a special supplement of COVID-19 in early April 2020, which addressed various issues in relation to management of COVID-19 and neurological disorders. The special issue included consensus statements on management of various neurological disorders and care related points. At ground level in routine neurology care the scene was dramatically changing minute by minute. The emergency departments were filling up with COVID19 patients and it appeared as if all the neurological emergencies have ‘vanished’ – which ended up being like a calmness of ‘eye of the hurricane’, before it hit us. The pattern and ‘ease’ of neurological practice has significantly changed with masks, face shields, personal protective equipment (PPE) kits and whole attire changing from a formal dressing to “Scrub suit” / “PPE suits” taking the forefront. This has definitely drained down a significant energy and amount of work output, but it appears like this will become a new norm for near future. Another interesting change has been the raise in tele consults / video consults. The medical practicing laws were quickly amended to accommodate the requirement of telemedicine. COVID19 has been a blessing in disguise for the telemedicine and this has become a main stay for most of the stable follow-up patients, albeit everyone does miss the personal/social touch with in-person consults.
2. Have you seen many people whom you were concerned had neurological complications of COVID19 infection? What are the most common neurological manifestations of COVID19 in your region?
COVID19 pandemic has made every speciality to gear up for its care. Most of us are working in regular COVID19 care which caters beyond neurological issues. The neurological manifestations of COVID19, which I have seen can be considered as those primarily related to COVID-19 infection, secondly to worsening of pre-existing neurological disorders due to COVID19 and finally those due to psychological effects of COVID19 breakout. The core neurological issues related to COVID19 included primarily thrombotic events in the form of acute ischemic events, cerebral venous sinus thrombosis in people, in whom no other risk / aetiologies could be pointed out. In addition, encephalitis / encephalopathy presentations were also seen in patients with COVID19. Many patients with severe COVID19 infections were reviewed for neurological consults and considered to have encephalopathies secondary to systemic COVID19 infection. The second set of problems was people with pre-existing neurological disorders like myasthenia gravis, multiple sclerosis, parkinsonism coming with acute worsening on a background of COVID19 infections. The third set of people were those who were not directly infected with COVID19, but with trauma of separation, quarantine, fear of not able to reach out to their doctors, limitation of social life leading to worsening of neurological symptoms especially with those of Parkinsonism disorders and dementia.
3. What are your main concerns for the future in regard to COVID19? What do you think are the key measures and contingency plans necessary to ensure high quality care for people living with neurological diseases during this pandemic? (read further)
Parkinson’s Disease challenge and advise collage from Doctors across India
#PDchallenge was initiated on July 22nd 2020 on the occasion of World Brain Day to create awareness about Parkinson’s Disease. The challenge included, showing various activities with a theme to win over Parkinson’s Disease. It included videos of patients, caregivers, friends, relatives, movement disorder specialists, neurologists, neurosurgeons, therapists, researchers from across the globe.
The following collage video shows the various Movement Disorders specialists, Neurologists, Neurosurgeons, researchers taking part in the #PDchallenge, released on August 15, 2020. This matches with the essence of ‘Mile Sur Mera Tumhara‘ theme of Unity in diversity theme song launched on August 15th 1988.
World Brain Day – #PDchallenge
#PDchallenge
Lets Shake the Parkinson’s Disease
World Brain Day 2020
#Parkinsons
Every year July 22nd is commemorated as WORLD BRAIN DAY. Annually one disorder will be highlighted to increase the awareness of the disorder. World Brain Day 2020 is dedicated to raising awareness for Parkinson’s Disease, a neurodegenerative brain disorder affecting more than 70 lakh people of all ages worldwide. This year, World Federation of Neurology and International Parkinson and Movement Disorder Society have joined together to end #parkinsons.
In this context, here in India, we are doing an active Parkinson’s Disease awareness campaign in the form of #PDchallenge. The challenge is open to all patients, caregivers, friends, health care workers and everyone across. The primary goal is to create awareness about Parkinson’s Disease. Please do a brief video about your active movements or agility and challenge your family members, friends, colleagues to show their agility. Come lets create awareness about Parkinson’s disease and remove the myths about it. Let’s create awareness by challenging our friends and relatives
10 things about Parkinson’s Disease for this World Brain Day:
- Parkinson’s Disease is neurodegenerative disease affecting the brain
- More than 70 Lakh people of all age groups affected by Parkinson’s Disease Worldwide.
- Parkinson’s Disease classically causes Slowness, Stiffness, Tremors and Balance problems.
- Mood changes, Anxiety, Depression, reduced smelling ability, Sleep disturbances, Urinary issues, Constipation, can also be affected.
- The Scare of the name “PARKINSON’S DISEASE”, make many people to loose hope in life.
- Parkinson’s disease is treatable
- People affected with Parkinson’s disease can lead a near normal quality of life.
- Good treatment options are available including mediations, injections and surgeries.
- Active life style and Exercises form the most important part of management of Parkinson’s Disease.
- Come on the World Brain Day, “Lets Shake the Parkinson’s”