Unveiling the Groundbreaking Solution for Parkinson’s Freezing of Gait
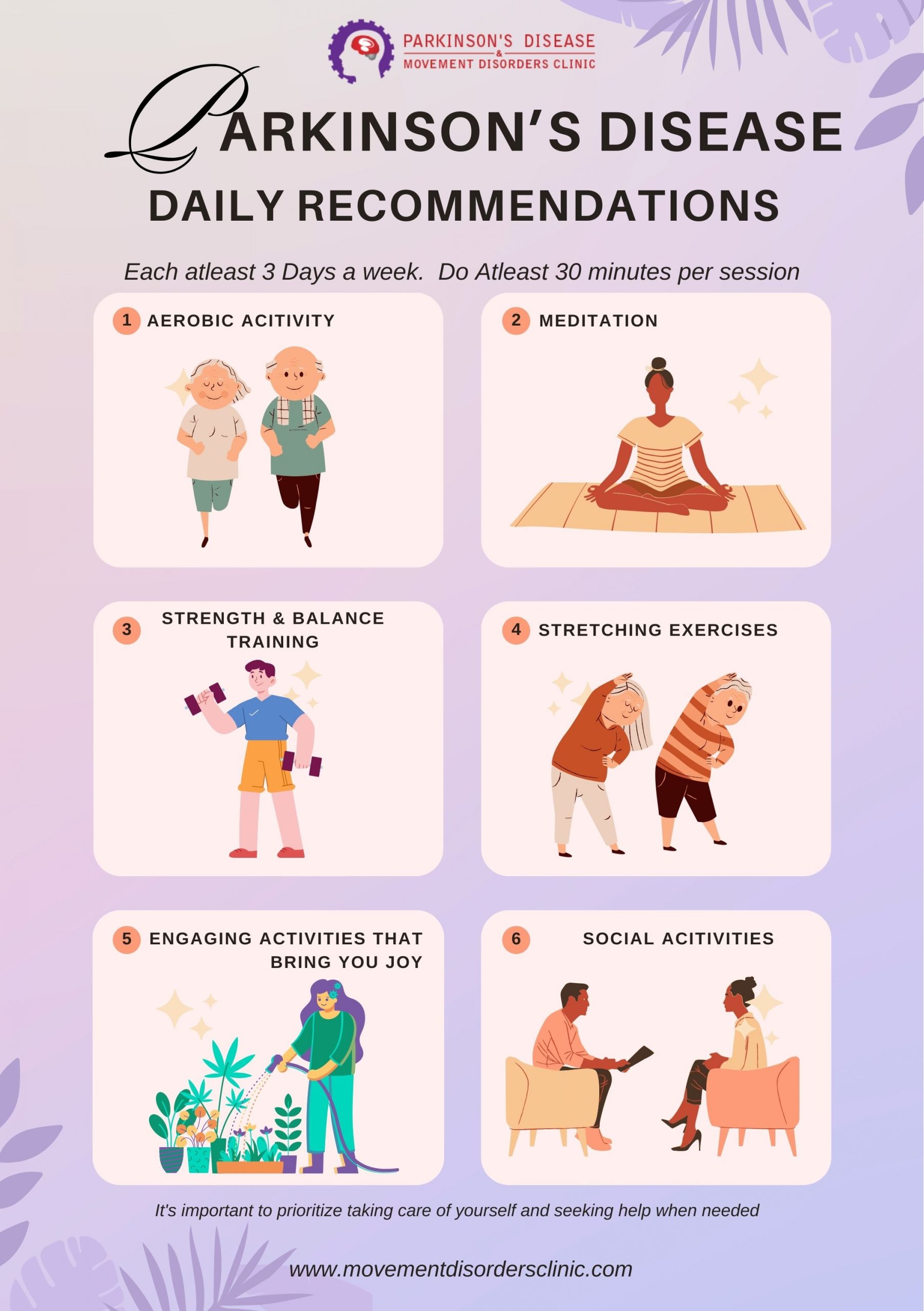
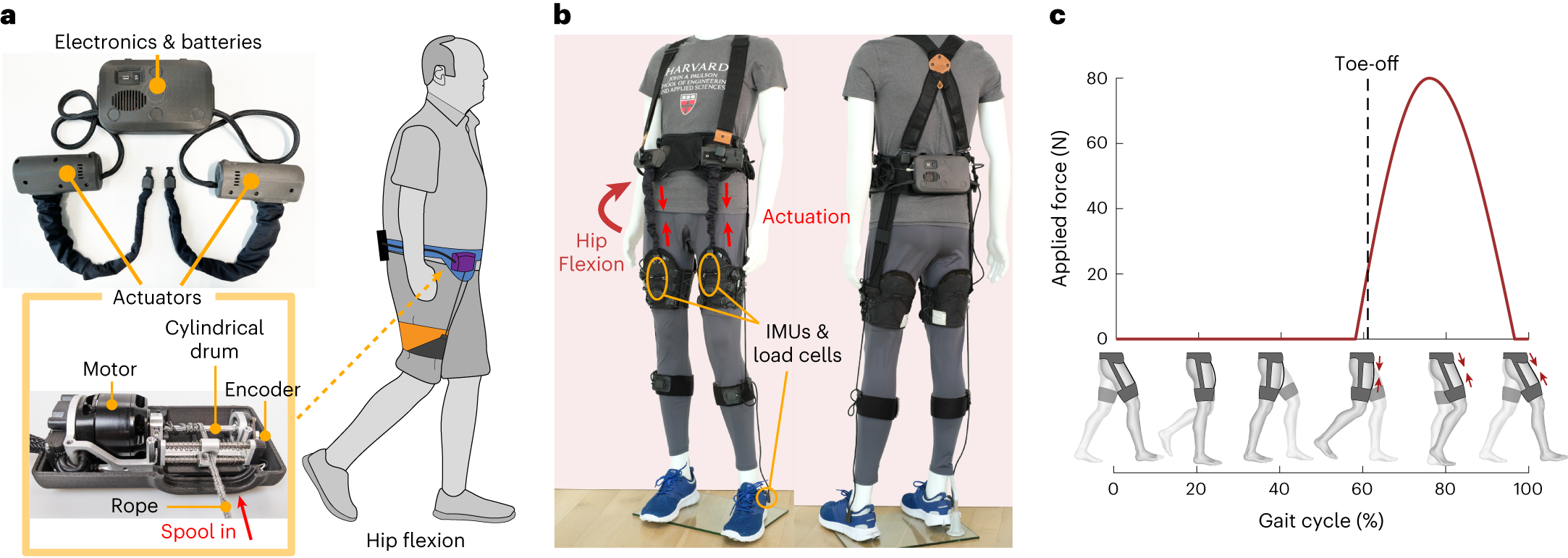
Parkinson’s disease affects over 9 million people worldwide and causes “freezing of gait,” which is one of the most debilitating symptoms. Recent research from the Harvard John A. Paulson School of Engineering and Applied Sciences and the Boston University Sargent College of Health & Rehabilitation Sciences has developed a soft, wearable robot that gently assists the wearer’s hip movement, enabling longer strides and eliminating freezing episodes indoors. The wearable garment uses cable-driven actuators and sensors, generating assistive moments in concert with biological muscles. The device’s impact was immediate, and the participant was able to walk without freezing indoors, and even outdoors, he experienced only occasional episodes. The device has the potential to deepen our understanding of gait freezing, a phenomenon that remains poorly understood. This soft robotic device offers a ray of hope for Parkinson’s patients worldwide, paving the way for further research into soft robotics and their potential to improve the lives of individuals grappling with this debilitating disease.
The study titled “Soft robotic apparel to avert freezing of gait in Parkinson’s disease” has been published in Nature Medicine (January 2024). The key findings of the study include:
- The soft robotic garment gently assists the wearer’s hip movement, enabling longer strides and eliminating freezing episodes indoors.
- The device’s impact was immediate, and the participant was able to walk without freezing indoors, and even outdoors, he experienced only occasional episodes.
- The study involved a 73-year-old man with Parkinson’s disease, who, despite undergoing surgical and pharmacologic treatments, experienced frequent and debilitating freezing episodes, leading to frequent falls and reduced mobility.
- The device’s sensors collected motion data and generated assistive forces in sync with muscle movement, effectively reducing freezing episodes.
- The study’s results offer a ray of hope for Parkinson’s patients worldwide, paving the way for further research into soft robotics and their potential to improve the lives of individuals grappling with this debilitating disease.
These findings support the potential of soft robotic devices in addressing the challenges faced by Parkinson’s patients, particularly in mitigating the effects of freezing of gait.
What is Freezing of Gait?
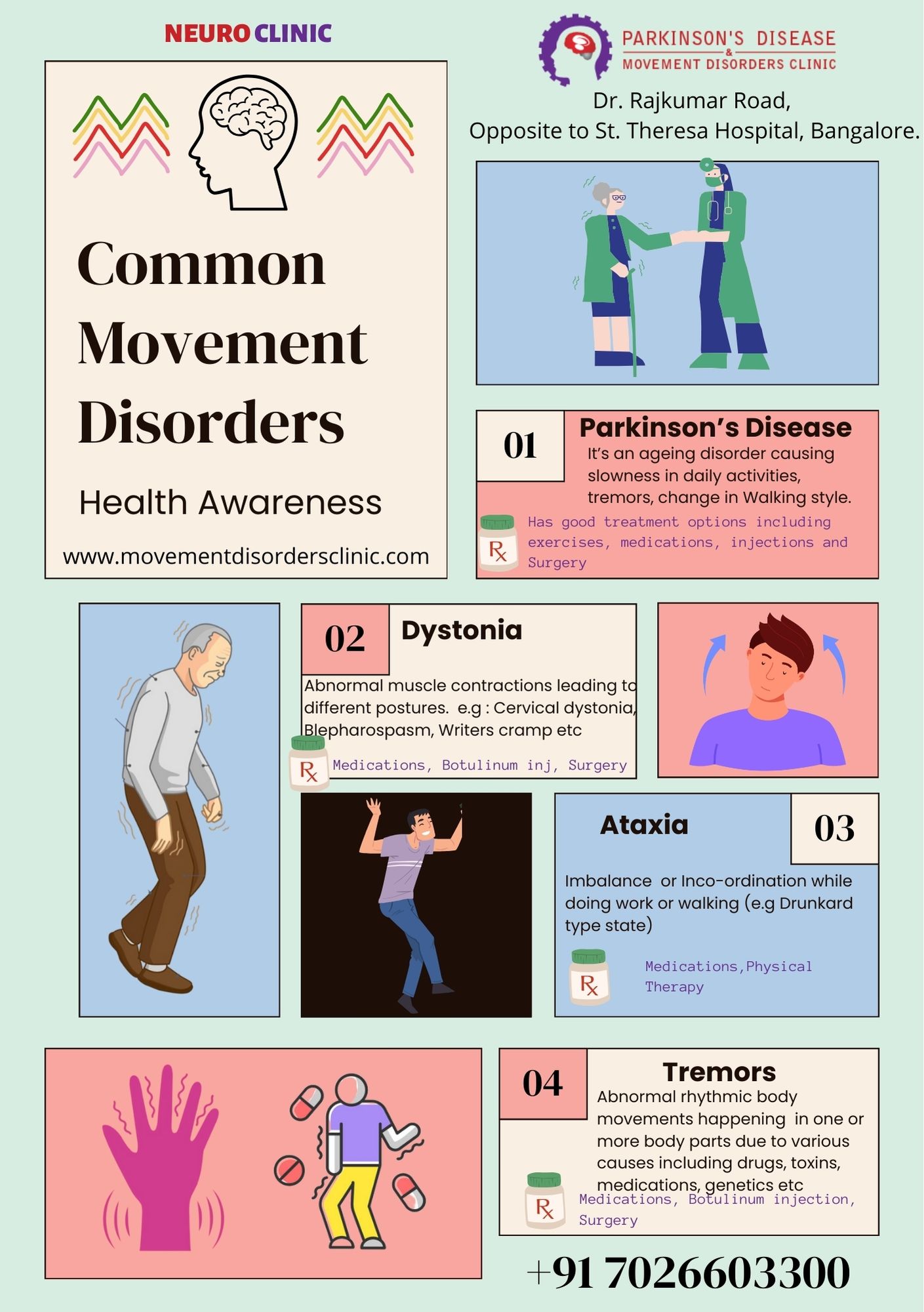
Freezing of gait is a common, disabling symptom of Parkinson’s disease (PD), but the mechanisms and treatments of FOG remain great challenges for clinicians and researchers. Freezing of gait (FOG) is defined as a brief, episodic absence or marked reduction of forward progression of the feet despite the intention to walk. During a freezing episode, a person with PD may feel like their feet are stuck in place, or glue to the ground. Freezing may also affect other parts of the body or speech. Some people are more likely to have freezing episodes than others. Freezing may occur when the person with PD is due for the next dose of dopaminergic medications. This is called “off” freezing — usually, until compensation strategies such as cueing is provided.
FOG is one of the most disabling yet poorly understood symptoms of Parkinson’s disease (PD). FoG is an episodic gait pattern characterized by the inability to step that occurs on initiation or particularly with perception of tight surroundings. This phenomenon impairs balance, increases falls, and reduces the quality of life. The exact cause of FOG is not known, but it is thought to be related to the degeneration of the basal ganglia, which is responsible for controlling movement.
FOG is not unique to PD and can also occur in other neurological conditions, such as, Higher Gait Disorders (HGD), multiple system atrophy (MSA), progressive supranuclear palsy (PSP), and corticobasal degeneration.
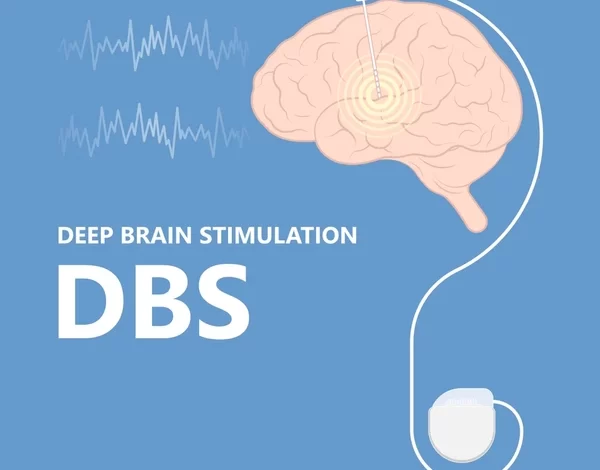
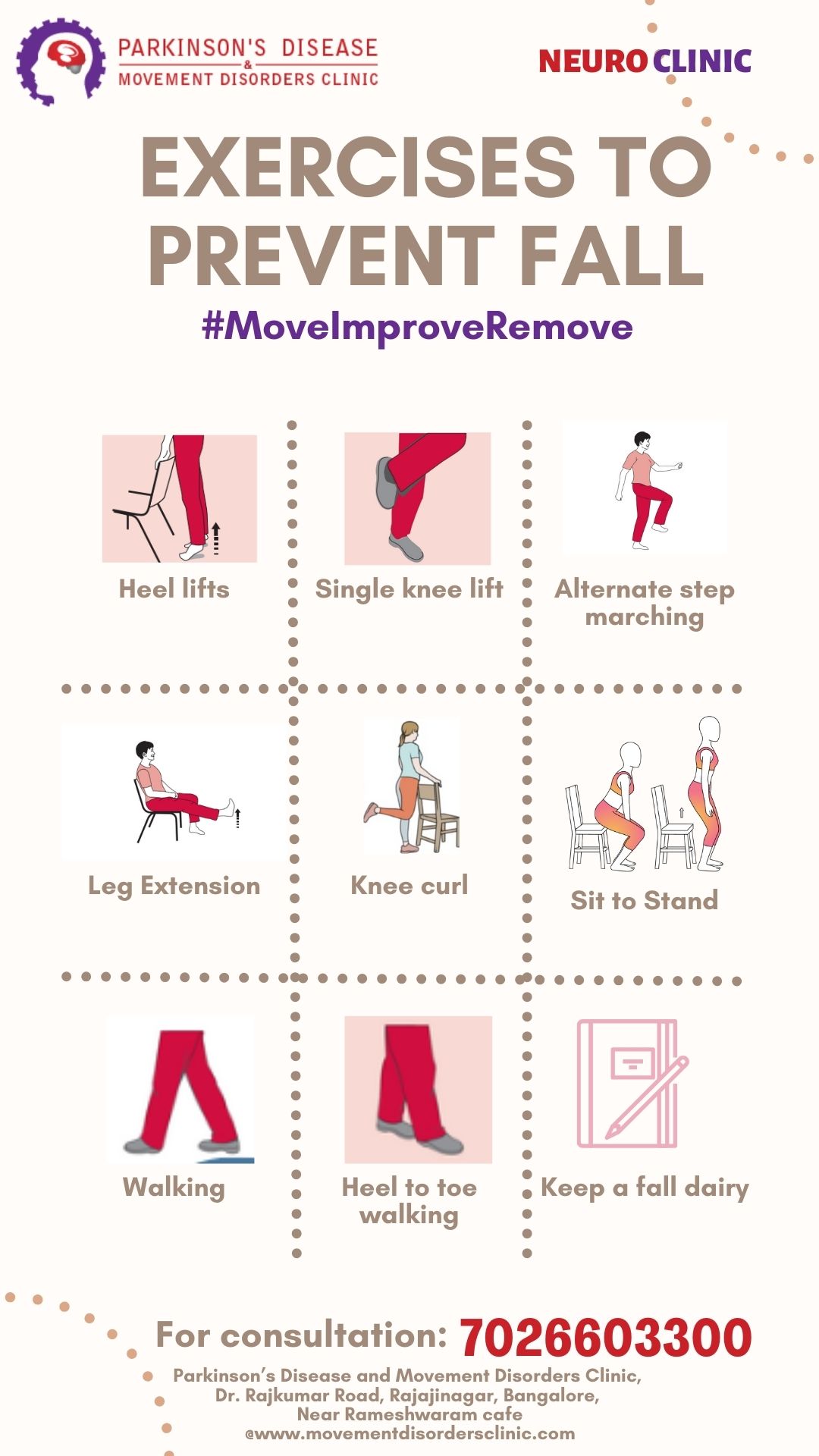
There are several treatment options for FOG, including pharmacological, surgical, and behavioral therapies. Pharmacological treatments include levodopa, dopamine agonists, and monoamine oxidase inhibitors. Surgical treatments include deep brain stimulation (DBS) and lesioning of the subthalamic nucleus (STN) or globus pallidus internus (GPi) with variable / suboptimal benefits for exclusive FOG. Behavioral therapies include cueing, which involves providing visual or auditory cues to help the patient initiate movement, and physical therapy, which can help improve balance and gait.
In recent years, researchers have developed a soft, wearable robot designed to combat freezing of gait in Parkinson’s patients. Worn around the hips and thighs, this innovative robotic garment gently assists the wearer’s hip movement, enabling longer strides and eliminating freezing episodes indoors. The device’s sensors collected motion data and generated assistive forces in sync with muscle movement, effectively reducing freezing episodes. The device’s impact was immediate, and the participant was able to walk without freezing indoors, and even outdoors, he experienced only occasional episodes.
In conclusion, FOG is a common and debilitating symptom of Parkinson’s disease that can also occur in other neurological conditions. The exact cause of FOG is not known, but it is thought to be related to the degeneration of the basal ganglia. There are several treatment options for FOG, including pharmacological, surgical, and behavioral therapies. Recent research has also shown promising results with a soft, wearable robot designed to combat freezing of gait in Parkinson’s patients.
Reference:
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8233405/
- https://translationalneurodegeneration.biomedcentral.com/articles/10.1186/s40035-020-00191-5
- https://www.nature.com/articles/s41591-023-02731-8
- https://www.thebrighterside.news/post/revolutionary-soft-robotic-exosuit-offers-hope-for-9-million-parkinson-s-patients-worldwide