Myths and Truth About Nanavathi Hospital Parkinson Injection Video
A Video about Parkinson’s disease patient being treated with apomorphine injections at Nanavathi Hospital , Mumbai became an social media craze in early 2019 (well known as Nanavati hospital Parkinson injection ). The video shows an dramatic improvement, which has made everyone to think that this is a cure for Parkinson’s disease. Thousands of Parkinson’s disease patients / caregivers thronged hospitals to find out about this therapy. Even medical fraternity were perplexed about this, and what was being conveyed. As a medical fraternity, we do know that till now there is NO CURE for parkinson’s disease currently. There are good treatments available for Parkinson’s disease including medications, injections and surgeries. Apomorphine is usually used as treatment option in moderately advanced Parkinson’s disease. The video shows basically an improvement seen after the injections, which could be similar to levodopa tablets or DBS. What it missed out on telling was this response would last only for about 60-90 minutes and this is only an symptomatic therapy.
As this video is popping up seasonally, this section would give an idea about Apomorphine and remove the myths around it.
Nanavati Hospital Parkinson Injection Video showing dramatic improvement
Dr Prashanth LK responding to Nanavathi Parkinson Injection Video
Facts about Apomorphine Injection Therapy for Parkinson Disease
FAQ about apomorphine injections
What is Apomorphine?
Apomorphine is a medication which is classified under “Dopamine Agonists”. This means it works towards increasing dopamine levels in the brain. Other medications under this category include Pramipexole, Ropinirole,etc.
Is Apomorphine similar to Morphine and causes addiction?
Apomorphine is derived from Morphine (Apo means “from”). It is produced by combining Morphine with acids like Hydrochloric acid at high temperatures. By this process, Morphine loses all its properties and a complete new chemical is formed. The chemical name of apomorphine is (C17H17NO2) and is significantly similar to Dopamine.
When was Apomorphine discovered? What are the conditions where Apomorphine is used?
Apomorphine was discovered in 1845. Since then it has been used in various medical conditions like :
i. Vomit inducing agent in poisoning patients,
ii. Sleep inducing agent,
iii. Anesthesia,
iv. De-addiction purposes
v. Respiratory distress disorders
vi. Sexual dysfunction
vii. Movement Disorders (Parkinson’sDisease)
How does apomorphine help in Parkinson’s disease?
In Parkinson’s disease patients, there is reduction of the brain chemical – Dopamine. Apomorphine increases the levels of dopamine and hence improvement in Parkinson’s symptoms.
Since when Apomorphine is used in management of Parkinson’s Disease?
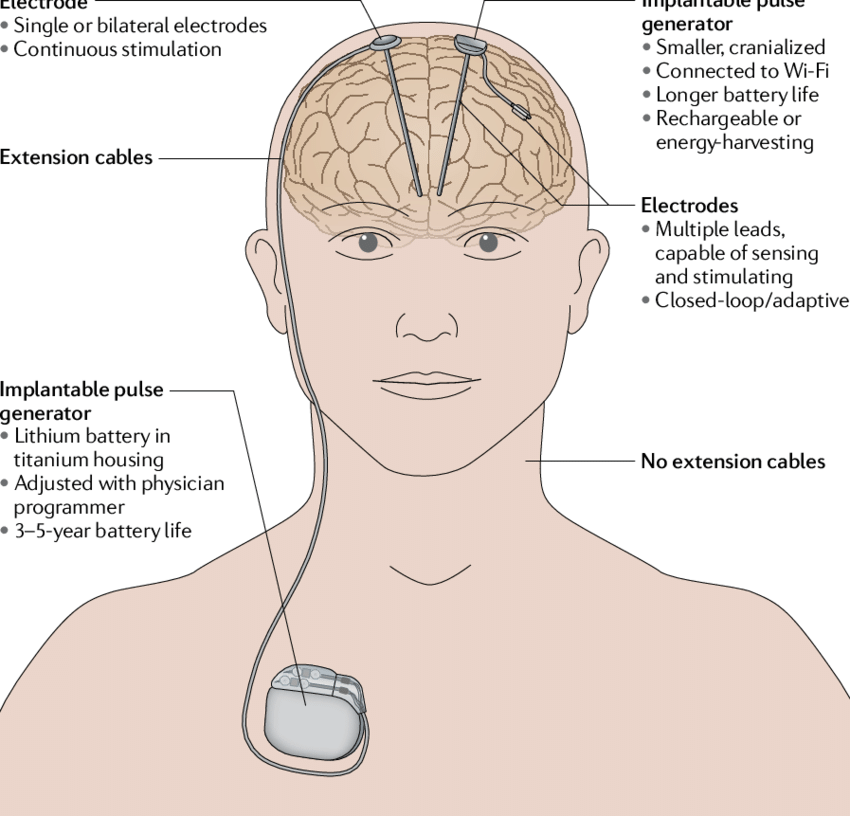
The first use of Apomorphine for Parkinson’s disease is around 1935. Since then it has been used in various studies. Its utilization was not prominent in early years due to nausea/ vomiting issues. With introduction of domperidone to reduce the side effects of Apomorphine, in 1970’s apomorphine utilization has dramatically increased and since last 20 years it is one of the options for advanced therapies for Parkinson’s Disease along with Deep Brain Stimulation (DBS) surgery and Levodopa-Carbidopa Intestinal gel (LCIG).
What are the different formulations, in which Apomorphine is available currently?
Apomorphine is primarily marketed in the form of Injections. However, tablet formulations are also available. There are research studies going on for newer delivery methods with better patient adaptation
What is the advantage of Apomorphine injections as compared to oral levodopa tablets used for Parkinson’s Disease?
We all know that as Parkinson’s disease progress, the duration of benefits of oral levodopa tablets start reducing and people will also start to have erratic responses. Sometimes the oral medications does not work or take too long to work as they are not absorbed properly in our gut (Stomach, duodenum). This is due the changes happening in our gut due to progression of Parkinson’s disease. Apomorphine, which is taken in injection formulation, bypassess the stomach absorption and hence its limitations. This bypassing helps to overcome the limitation of medications and gives quick and predictable benefits.
What are Apomorphine Rescue Injections? How long does it take to work and last for?
Apomorphine rescue injections are “emergency injections” which can be carried by patients in their pockets like “Insulin Injection pens”. If at any time, any Parkinson’s disease patient develops severe slowness, he can take subcutaneous injections similar to insulin injections. This apomorphine injection usually starts working within 5-10 minutes and gives quick and predictable relief. This whole beneficial effect lasts for about 60-90 minutes, helping people to tide over acute worsening. Hence called Rescue injections.
What is Apomorphine Pump Therapy?
In advanced Parkinson’s disease, people who are in need of taking medications very frequently and limited by benefits of oral therapy (like ON-OFF phenomenon, dyskinesia) are suggested for advanced Parkinson’s disease therapies. Apomorphine pump therapy is an advanced Parkinson’s disease therapy. It involves slow release of apomorphine throughout the day and hence providing stable, predictable benefits. It is somewhat similar to Insulin Pump therapy used by diabetes patients.
Are Apomorphine Pump therapy available in India?
Yes, currently two different generations of Apomorphine pumps are available in India. These products are in use in India since 2019. These are supplied by – Rusan Pharamceuticals and Ever Pharma (Celera India)
Can anyone with Parkinson’s Disease take Apomorphine?
Apomorphine is used in specific stages of Parkinson’s disease to get desired benefits and improve quality of life. Your treating doctor would be able to tell whether you would benefit from Apomorphine therapy.
In the initial phase Apomorphine is used to assess whether the givenParkinson’s disease / Parkinsonism patient would be having benefits with levodopa therapy. This is called the “Apomorphine ResponseTest (ART)”.
In mid-phase of Parkinson’s disease, Apomorphine is used as emergency medications to give quick benefits when certain dosages of levodopa are not working due to various causes. This is called as “Rescue Therapy”
In moderately advanced Parkinson’s Disease, Apomorphine is used in continuous injections in the form of “ApomorphinePumpTherapy ” to over come motor fluctuations (ON – OFF phenomenon) and Dyskinesias.
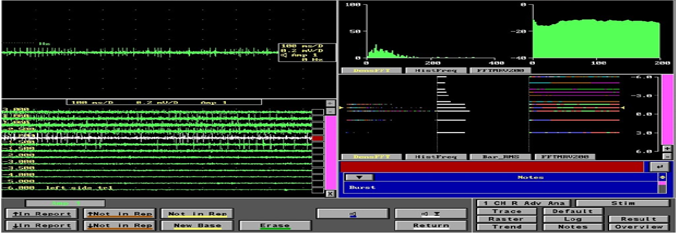
What is an Apomorphine Response Test(ART)?
Apomorphine Response test or ART is a test to see whether your clinical symptoms improve with Apomorphine. This is done as an elective procedure, where in certain blood tests are done prior to testing. You would also be given “domperidone” tablets to reduce the side effects of Apomorphine. During ART, you would be asked to come in the morning without taking any levodopa and you would be assessed by giving different dosages of Apomorphine injections (usually ranging from 1mg to 6mg). The whole process may last from 90mins to 4-5 hours depending on response and side effects. Your treating doctor/team, will explain about this in detail. If there is a good response to ART, then you can be recommended for rescue therapy OR pump therapy as required.
What is Apomorphine Pump Therapy?
Apomorphine Pump therapy involves slow and continuous release of Apomorphine using a small pump, which can be carried in the pocket or sling bag or belt attachment. The continuous slow release of Apomorphine gives a predictable response throughout the day.
This takes away the side effects of excess medications and has the ease of quick adjustments. Usually pump therapy is given for about 10-16 hrs in a waking day period. However, in some cases night time use is also recommended.
What are the advantages of Apomorphine pump therapy in Parkinson’s Disease?
The advantages of Apomorphine pump therapy include:
i. It gives predictable responses
ii. Dosages can be easily modified as required
iii. No upfront cost like in DBS or LCIG gel therapies
iv. It is also used in patients in whom DBS is contraindicated and has shown good consistent benefits.
v. It has beneficial effects on cognitive function and can be used in people who are having mild to moderate cognitive impairment (where DBS is contraindicated)
vi. It is used in patients with resistant axial symptoms (Camptocormia – bending spine posture) with good benefits.
vii. It is also used in patients in whom DBS effects are reducing over the period of time to give add on benefits.
viii. It can be used for resistant Restless legs syndrome
What are the disadvantages of Apomorphine Pump Therapy?
The disadvantages of Apomorphine are similar to that of Levodopa, Pramipexole, Ropinirole etc. Specific disadvantage of Apomorphine pump therapy include:
i. It has to be managed on a daily basis to start and stop. Some patients may require assistance for the same.
ii. Some people are scared of needle pricks, which is a hurdle for utilization.
iii. Some people feel it is clumsy to carry.
iv. Skin injection sites small nodules are formed. Albeit they are temporary and non-concerning, rarely they can get infected causing problems.
v. Some people continue to have disturbing side effects of nausea, vomiting, drowsiness, blood pressure fluctuations in spite of domperidone.
Most of the dropouts in Apomorphine pump therapy have been noted in the first few months due to adaptation required. However once accepted, people have been using it over many years, with consistent benefits.
Are there any studies Indian / International on benefits of Apomorphine therapies?
Apomorphine therapy has been well accepted therapy for Parkinson’s disease for the last 30+ years. This is categorized under advanced therapies for Parkinson’s disease along with DBS and LCIG. There have been many publications on benefits and long term outcomes of Apomorphine therapy from various countries including India. There are guidelines published by International Movement Disorders groups on who should use apomorphine therapies.
Is Apomorphine injections / therapy available everywhere across India?
Theoretically Apomorphine should be available everywhere across India easily. However as this is an advanced therapy and used in a certain set of Parkinson’s Disease, the ease of access is limited to these advanced movement disorders centers in India. Usually you would be guided on how to procure after therapy initiation. Most of the time they are delivered to each patient on a requirement basis, without any major logistical issues. Even during COVID times, the logistics were maintained and even dispatched to patients who were struck abroad due to lockdown.
Where should I contact for Apomorphine pump therapy?
Your treating doctor will be able to guide you to the nearest Parkinson’s Disease center, who specialize in apomorphine therapies. Please speak to your treating Neurologist / Movement Disorders Specialist for further details.
Resources and Further reading
1. Prashanth LK, Jaychandran R, Seetharam R, Iyer RB. Apomorphine: The Initial Indian Experience in Relation to Response Tests and Pumps. Ann Indian Acad Neurol. 2020 Jan-Feb;23(1):20-24. doi: 10.4103/aian.AIAN_428_19. Epub 2019 Dec 19. PMID: 32055117; PMCID: PMC7001430.
2. Kukkle PL, Garg D, Merello M. Continuous Subcutaneous Infusion Delivery of Apomorphine in Parkinson’s Disease: A Systematic Review. Mov Disord Clin Pract. 2023 Jun 26;10(9):1253-1267. doi: 10.1002/mdc3.13810. PMID: 37772305; PMCID: PMC10525070.
3. Metta V, Borgohain R, L Kukkle P, Mridula R, Agarwal P, Kishore A, Goyal V, Chaudhuri R. Subcutaneous apomorphine in advanced Parkinson’s disease and its use in Indian population. Ann Mov Disord 2020;3:145-55
4. Trenkwalder C, Chaudhuri KR, García Ruiz PJ, LeWitt P, Katzenschlager R, Sixel-Döring F, Henriksen T, Sesar Á, Poewe W; Expert Consensus Group for Use of Apomorphine in Parkinson’s Disease, Baker M, Ceballos-Baumann A, Deuschl G, Drapier S, Ebersbach G, Evans A, Fernandez H, Isaacson S, van Laar T, Lees A, Lewis S, Martínez Castrillo JC, Martinez-Martin P, Odin P, O’Sullivan J, Tagaris G, Wenzel K. Expert Consensus Group report on the use of apomorphine in the treatment of Parkinson’s disease–Clinical practice recommendations. Parkinsonism Relat Disord. 2015 Sep;21(9):1023-30. doi: 10.1016/j.parkreldis.2015.06.012. Epub 2015 Jun 17. PMID: 26189414.
5. Jenner P, Katzenschlager R. Apomorphine – pharmacological properties and clinical trials in Parkinson’s disease. Parkinsonism Relat Disord. 2016 Dec;33 Suppl 1:S13-S21. doi: 10.1016/j.parkreldis.2016.12.003. Epub 2016 Dec 13. PMID: 27979722.
6. Todorova A, Ray Chaudhuri K. Subcutaneous apomorphine and non-motor symptoms in Parkinson’s disease. Parkinsonism Relat Disord. 2013 Dec;19(12):1073-8. doi: 10.1016/j.parkreldis.2013.08.012. Epub 2013 Aug 29. PMID: 24051336.
7. Dafsari HS, Martinez-Martin P, Rizos A, Trost M, Dos Santos Ghilardi MG, Reddy P, Sauerbier A, Petry-Schmelzer JN, Kramberger M, Borgemeester RWK, Barbe MT, Ashkan K, Silverdale M, Evans J, Odin P, Fonoff ET, Fink GR, Henriksen T, Ebersbach G, Pirtošek Z, Visser- Vandewalle V, Antonini A, Timmermann L, Ray Chaudhuri K; EUROPAR and the International Parkinson and Movement Disorders Society Non- Motor Parkinson’s Disease Study Group. EuroInf 2: Subthalamic stimulation, apomorphine, and levodopa infusion in Parkinson’s disease. Mov Disord. 2019 Mar;34(3):353-365. doi: 10.1002/mds.27626. Epub 2019 Feb 4. PMID: 30719763.
8. Fernández-Pajarín G, Sesar Á, Ares B, Castro A. Evaluating the Efficacy of Nocturnal Continuous Subcutaneous Apomorphine Infusion in Sleep Disorders in Advanced Parkinson’s Disease: The APO-NIGHT Study. J Parkinsons Dis. 2016 Oct 19;6(4):787-792. doi: 10.3233/JPD-160886. PMID: 27662329.
9. Sesar Á, Fernández-Pajarín G, Ares B, Rivas MT, Castro A. Continuous subcutaneous apomorphine infusion in advanced Parkinson’s disease: 10-year experience with 230 patients. J Neurol. 2017 May;264(5):946-954. doi: 10.1007/s00415-017-8477-0. Epub 2017 Mar 31. PMID: 28364292.
10. Borgemeester RWK, van Laar T. Continuous subcutaneous apomorphine infusion in Parkinson’s disease patients with cognitive dysfunction: A retrospective long-term follow-up study. Parkinsonism Relat Disord. 2017 Dec;45:33-38. doi: 10.1016/j.parkreldis.2017.09.025. Epub 2017 Sep 29. PMID: 29032012.
11. Sesar Á, Fernández-Pajarín G, Ares B, Relova JL, Arán E, Rivas MT, Gelabert-González M, Castro A. Continuous subcutaneous apomorphine in advanced Parkinson’s disease patients treated with deep brain stimulation. J Neurol. 2019 Mar;266(3):659-666. doi: 10.1007/s00415-019-09184-5. Epub 2019 Jan 7. PMID: 30617907.
12. Menšíková K, Kaiserová M, Vaštík M, Nevrlý M, Kurčová S, Kaňovský P, Colosimo C. The long-term effect of continuous subcutaneous apomorphine infusions on camptocormia in Parkinson’s disease. Parkinsonism Relat Disord. 2020 Jun;75:14-16. doi: 10.1016/j.parkreldis.2020.05.015. Epub 2020 May 12. PMID: 32442812
Overall this Nanavati Hospital Parkinson injection video has been impressive in creating awareness about treatment options for people with Parkinson’s disease. Many people have equated Nanavati Hospital Parkinson injection video to be synonymous with cure for Parkinson’s disease, which is a misinterpretation of the video circulated, leading to lot of myths associated around this therapy. We hope our blog on Nanavati hospital Parkinson injection video gives an open insight into the indications, uses and limitations of this therapy and breaks down into some of the myths which are being interpreted from this video.