Diet for Parkinson’s: Unveiling the Current Science Behind Your Food Choices
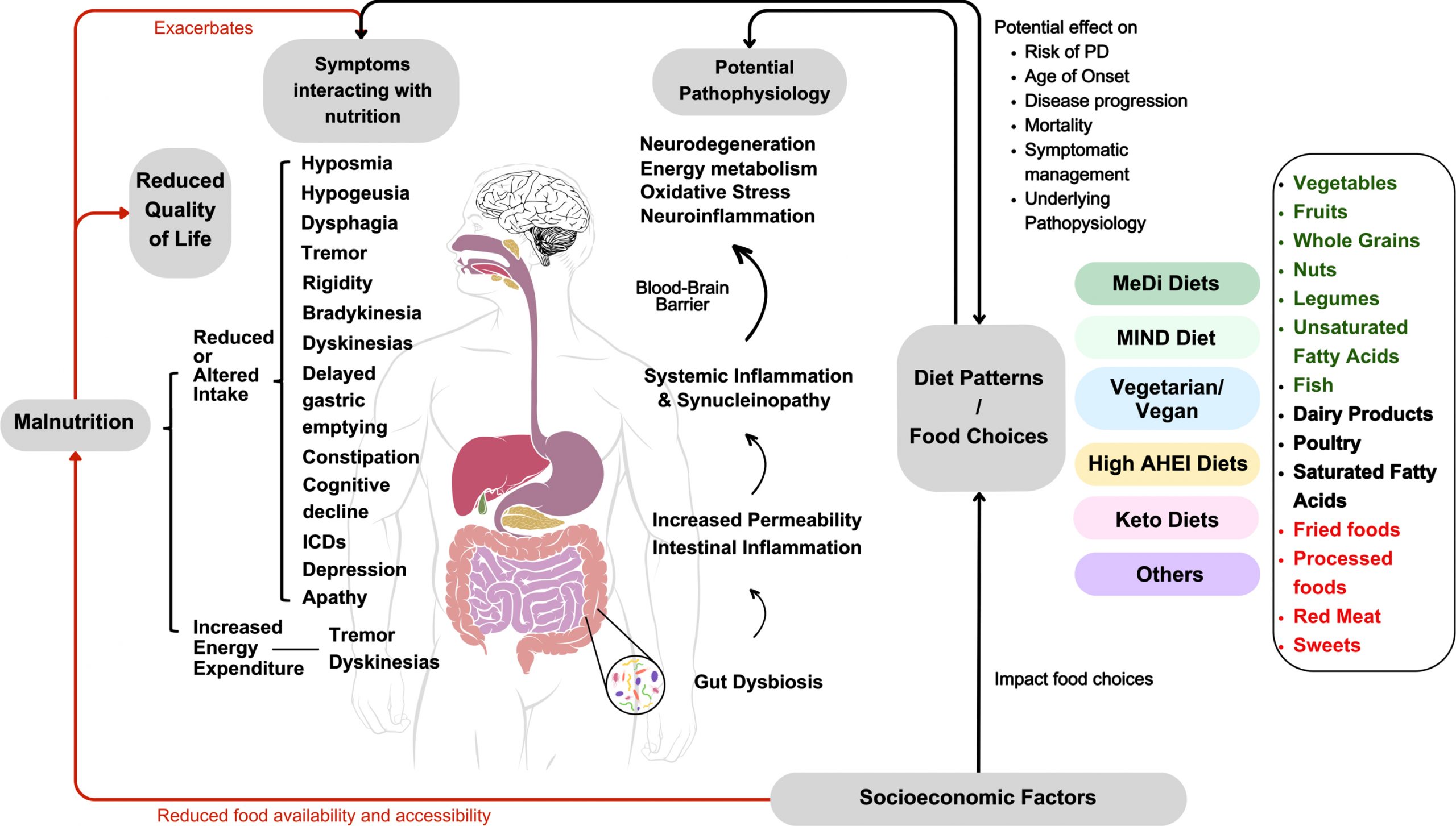
Parkinson’s disease (PD) is a common brain condition that affects many people worldwide and What is a right diet for Parkinson Disease is an enigma. Some studies have looked at how different diets might affect Parkinson’s Disease and found some interesting connections, but there’s still a lot we don’t know. We do know that many people with PD aren’t getting the right nutrients they need, which can make their health and how they feel worse. So, researchers are trying to figure out if changing what people eat or taking certain vitamins could help them feel better and slow down how fast PD gets worse (What’s the Best Diet for Parkinson Disease? ). This article will talk about what we know so far about how food and supplements might help people with Parkinson’s disease, and what we need to learn more about based upon a recent scientific publication in the Journal of Parkinson’s Disease by Kira Tosfesky.
Dietary Patterns

Mediterranean Diets
Mediterranean diets are all about eating lots of plant-based foods like veggies, fruits, whole grains, beans, and nuts. They also include fish and seafood, a bit of chicken, and some wine. But you eat less red meat, sweets, and sugary drinks. Studies from 2020 to 2023 found that following this diet could lower the risk of getting Parkinson’s disease (PD). One study even showed that men who followed this diet had Parkinson’s symptoms show up later, up to 8.4 years later. These diets are thought to help because they have lots of antioxidants and good fats that protect the brain. However, there haven’t been many big studies testing if this diet can really help people with Parkinson feel better.
MIND Diet
The MIND diet is a mix of the Mediterranean and Dietary Approaches to Stop Hypertension (DASH) diets, made to keep the brain healthy. It says to eat a lot of leafy greens, beans, and berries, but not so much cheese, butter, or margarine. One study found that following the MIND diet was linked to a lower risk of getting parkinsonism, a condition like Parkinson’s disease, and slower symptoms than following the Mediterranean diet. Another study showed that women who followed the MIND diet had Parkinson’s symptoms show up later, up to 17.4 years later. But we still need more research to know for sure if this diet can really help people with Parkinson’s feel better.
Vegetarian and Vegan Diets
Some studies suggest that societies where people mostly eat vegetarian or vegan diets have lower rates of Parkinson’s disease (PD). A study in the UK found that people who ate healthy plant-based diets had a lower risk of getting PD, while those who ate unhealthy plant-based diets had a higher risk. Another study tested a vegetarian diet on 16 patients with PD for 14 days and found that it helped improve their symptoms. But we still need more research to know if these diets can really help people with PD feel better.
Ketogenic diet
The ketogenic diet (KD) is a special diet that is high in fat and low in carbohydrates. This diet might help people with Parkinson’s disease (PD) because it provides a different type of fuel for the brain called ketones. Ketones can help the brain work better when the usual fuel, glucose, doesn’t work as well in PD. Some studies tested this diet on people with PD and found that it might help improve symptoms like movement problems and anxiety. However, some people had more tremors or stiffness when they started the diet, so we need more research to understand if the ketogenic diet is really helpful for everyone with PD.
Protein redistribution diets:
Changing when you eat protein might help people with Parkinson’s disease (PD) get more benefit from their medication. Protein-redistribution diets involve eating most of your protein at dinner and less during the day. Studies on these diets showed that they could reduce movement problems by 32–79% and help with other symptoms too. But some people worry that these diets might make you lose weight or muscle. So, more research is needed to understand if they’re safe and helpful for everyone with PD.
Food Groups

Dairy:
Eating a lot of dairy, like milk, cheese, and yogurt, might have different effects on Parkinson’s disease (PD). Some studies suggest that high dairy consumption could raise the risk of getting PD. However, the type of dairy matters too. Low-fat dairy seems to be linked more strongly to PD risk than full-fat dairy. Ice cream, yogurt, and cheese have been connected to faster PD progression. The reasons behind these connections are not fully understood, but it could be because of certain chemicals in dairy products or pesticides used in farming.
Alcohol:
The relationship between alcohol and PD is mixed. Some studies suggest that moderate alcohol intake might increase the risk of PD in men. But other research shows a U-shaped association, meaning both heavy drinkers and those who don’t drink at all might have higher risks. However, these findings might be influenced by other factors like smoking or personality traits. Some think that the antioxidants in alcohol could protect against PD, but more research is needed to understand how alcohol affects PD risk.
Caffeine:
Drinking coffee and tea with caffeine might help lower the risk of PD and slow down its progression. Caffeine seems to affect certain chemicals in the brain that are involved in PD. However, studies testing caffeine pills alone haven’t shown the same benefits. This suggests that other parts of coffee and tea might also play a role in protecting against PD.
PD-Specific Foods:
Some foods seem to affect how fast Parkinson’s disease progresses. Eating more fresh vegetables, fruits, nuts, fish, olive oil, and spices could slow down the disease. On the other hand, canned fruits and vegetables, fried foods, beef, and dairy products like ice cream and yogurt might make PD symptoms worse. These findings are based on what people with PD have reported, but more research is needed to understand how different foods affect the disease.
Nutritional Supplements

Vitamin D:
Many studies have found that people with Parkinson’s disease (PD) often have low levels of vitamin D. This can affect how severe their symptoms are and even increase the risk of falls. Vitamin D plays an important role in the brain, especially in the area affected by PD. Some studies have tested giving extra vitamin D to people with PD, but so far, it doesn’t seem to have a big effect on symptoms. However, it’s still important for people with PD to make sure they get enough vitamin D to keep their bones healthy.
Vitamin E and Omega-3 Fatty Acids:
Vitamin E and omega-3 fatty acids are thought to help with PD because they have antioxidant and anti-inflammatory properties. Some studies have found that taking these supplements can improve PD symptoms and reduce inflammation in the body. Fish oil, which contains omega-3 fatty acids, seems to slow down PD progression according to some studies. But more research is needed to confirm these benefits.
Vitamins B6, B9, and B12:
People with PD often have high levels of a substance called homocysteine in their blood, which can be harmful. Vitamins B6, B9 (folate), and B12 can help lower homocysteine levels. Some studies suggest that taking these vitamins might help prevent or slow down PD, but more research is needed to be sure.
Other Vitamins:
Vitamins B1 (thiamine) and C don’t seem to have a big effect on PD risk, but they might help with symptoms. Thiamine deficiency has been linked to memory problems in PD, while vitamin C might help the body absorb PD medications better.
Fiber, Prebiotics, and Probiotics:
Gut problems are common in PD, so some researchers are looking at how fiber, prebiotics, and probiotics might help. Probiotics, in particular, seem to improve PD symptoms and mood in some studies, but more research is needed to understand their effects fully.
Mucuna Pruriens:
Mucuna pruriens is a plant that contains levodopa, the main medication used to treat PD. Some studies suggest that it might work as well as synthetic levodopa in controlling PD symptoms.
Conclusions
Conclusions:
Diet for Parkinson disease is a common daily enigma for both people with PD and health care professionals. Understanding the role of nutrition in Parkinson’s disease (PD) is crucial for patients, researchers, and doctors. While many studies show a link between diet and PD, there’s a lack of high-quality research, making it hard to give clear recommendations. Challenges in studying nutrition in PD include differences in people’s diets, difficulty in measuring food intake accurately, and the need for long-term studies to see if diets can change the course of the disease. Despite these challenges, some diets like the Mediterranean and MIND diets seem promising for PD. However, more research is needed to confirm their benefits. Certain supplements, like vitamin E and omega-3 fatty acids, may also help with PD symptoms, but more studies are necessary. Other dietary factors, such as alcohol and dairy, have mixed evidence regarding their impact on PD risk and progression. While probiotics show promise in managing PD symptoms, more research is needed to understand their effectiveness fully. Overall, nutrition plays a crucial role in PD management, but more research is needed to provide clear guidelines and overcome barriers to dietary changes for patients.
Reference Publication :
Tosefsky, Kira N. et al. ‘The Role of Diet in Parkinson’s Disease’. 1 Jan. 2024 : 1 – 14.